Use of metformin according to renal function in patients with type II diabetes
2 Department of Biochemistry, JSS Medical College, Academy of Higher Education and Research, Mysuru, Karnataka, India, Email: bnmurthy24@gmail.com
3 Department of Forensic Medicine and Toxicology, University of Benghazi, Libya, Email: tahanihuria@gmail.com
Received: 07-Dec-2020 Accepted Date: Dec 23, 2020; Published: 31-Dec-2020
Citation: Salem SR, Beeraka NM, Roaeid RB, et al. Use of metformin according to renal function in patients with type II diabetes. Clin Pharmacol Toxicol Res. 2021;4(1):1-6.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The most widely prescribed hypoglycaemic drug worldwide is metformin. Since many diabetic patients have Chronic Kidney Disease (CKD), its use is often reduced by clinicians due the risk of Lactic Acidosis (LA) as warned by US Food and Drug Administration (FDA). Widespread use of metformin will simplify the management of type II diabetes mellitus with lower incidences of hypoglycaemia. The FDA is finally requiring labelling changes about recommendations to consent the use of metformin in patients with reduced kidney function. However, there are several clinical conditions that are considered as contraindications to the use of metformin among patients with type II diabetes mellitus. The clinical conditions are renal dysfunction, Congestive Heart Failure (CHF), metabolic acidosis, and impaired hepatic function. In this paper work, the most common form of drug used by most of the patients was metformin. Previous studies showed that CHF is the most common contraindication of metformin, while in this paper work chronic renal impairment is the most frequent contraindication of metformin in type II diabetes according to renal function test. Renal impairment can be defined according to Estimated Glomerular Filtration Rate (EGFR). The use of metformin is absolutely contraindicated in patients with severe CKD (EGFR<30 ml/min/1.73 m2). Therefore, patients with moderate CKD (EGFR 30-59 ml/min/1.73 m2) are eligible to receive metformin. This paper work identified the prescription pattern of metformin across CKD stages in diabetic patients. Patient with EGFR<30 mL/min/1.73 m2 using metformin, impairments were severe enough to avoid metformin use. Patients with EGFR 30-60 mL/min/1.73 m2 and their ages above 60 years with non-controlled Fasting Blood Sugar (FBS), glycated haemoglobin (HbA1C), hypertension and ischemic heart disease are eligible to receive metformin. As metformin is rarely the sole cause of LA, renal function should be monitored closely in type II diabetic patients using metformin.
Keywords
Metformin; Patients with type II diabetes mellitus; EGFR
Aim of the Study
This paper work aimed for investigation of the prevalence nature of metformin therapy contraindications among type II diabetic patients at Benghazi Diabetic Centre, Libya, also for exploration of metformin prescription practices in relation to EGFR level and likewise, for the examination of relationship between EGFR, age, gender and duration of diabetes.
Introduction
Diabetes is a long-term condition that causes a person’s blood sugar level to become too high [1]. Chronic diabetes conditions include type I and type II diabetes [1]. Type II diabetes is due to a progressive insulin secretory defect on the background of insulin resistance [2]. It is the more common type of diabetes which can develop at any age [1]. Though it is more common in people older than 40s, ranging from predominantly insulin resistance with relative insulin deficiency to predominantly an insulin secretory defect with insulin resistance [1,3]. It accounts for 90%-95% of those with diabetes, previously referred as non-insulin-dependent diabetes, or adult-onset diabetes [1,3]. It encompasses individuals who have insulin resistance and usually have relative (rather than absolute) insulin deficiency [4]. At least initially, and often throughout their lifetime, those individuals do not need insulin treatment to survive. There are probably many different causes of this form of diabetes. Although the exact cause is not known, there are probably many different causes of this form of diabetes [5]. Although it’s believed that genetic and environmental factors play a role in the development of type II diabetes. Being overweight is strongly linked to the development of type II diabetes, but not everyone with type II is overweight. The longer patients have diabetes and the less controlled their blood sugar the higher risk of complications [5]. Eventually, diabetes complications may be disabling or even life-threatening if not treated probably [6]. It includes heart diseases, nephropathy, neuropathy, hearing problem, psychological diseases, skin problems, gangrene and etc. The cornerstone of type II diabetes management is a healthy diet, increased physical activity and maintaining a healthy body weight [6]. Oral hypoglycaemic drugs and insulin injection are also frequently prescribed to help control blood glucose levels [6].
Metformin (biguanide)
Metformin is an oral hypoglycaemic agent of the biguanide class that lowers blood glucose level mainly by decreasing hepatic glucose production and improving insulin sensitivity of the peripheral tissues by increasing peripheral glucose uptake and utilization [7]. It leads to a reduction in FBS levels and HbA1c. Metformin is not associated with a risk of hypoglycaemia; because it does not stimulate endogenous insulin production, in contrast to other antidiabetic drugs [7]. Metformin was approved by the U.S. FDA in 1994, and it is generally recommended as the first-line pharmacological agent in management guidelines for patients with type II diabetes mellitus because of its low cost, safety, and association with a reduction in the risk of cardiovascular events [8,9]. However, it is not metabolized and it is excreted in the urine unchanged and renal impairment may cause the accumulation of metformin leading to an elevated metformin concentration, and this has been proposed to lead to lactic acidosis [10,11].
Chronic kidney disease (ckd)
CKD is a worldwide recognized public health issue affecting 3-16% of the population in over the world [7]. CKD is defined as histopathological kidney damage and/or decreased kidney function, lasting more than 3 months. Kidney damage usually precedes alterations in function [11]. The kidney structure is considered to be affected when one or more markers of kidney damage are present, such as proteinuria and/or abnormalities detected by histology or non-invasive imaging [11,12]. The histopathological features of CKD are tubulointerstitial fibrosis, tubular atrophy, cellular infiltration, and glomerulosclerosis [13,14]. The most prominent functional parameter of the kidney is the Glomerular Filtration Rate (GFR), which equals the total amount of fluid filtered through the glomeruli per unit of time [13,14]. The Kidney Disease Outcomes Quality Initiative (KDOQI) of the National Kidney Foundation (NKF) divided CKD into five stages, regardless of underlying causes. Decreased EGFR of less than 60 mL/min/1.73 m2 is defined by the current international guidelines as CKD [13-15]. When the EGFR is less than 15 mL/min/1.73 m2, the final stage of renal failure, at which kidney function is no longer sufficient to meet the body’s need, is reached. In developed countries, age, diabetes, hypertension, cardiovascular disease and obesity, are the leading causes of CKD [13-15].
Patients and Methods
A cross-sectional study, a purposive sample was recruited. Patients attending Benghazi Diabetic Centre-Benghazi, Libya and data were collected on daily visits over a period of 6 months. Patient`s age and sex were included and detailed medical history was taken from the patient. FBS, HbA1C, renal function test, EGFR, and EPI-CKD equation was used to calculate EGFR electronically. All the patients who are included in this study have registration card and agreed to participate.
Ethical considerations
This project was conducted according to medical research ethics, the patients were informed about the study, a verbal consent was freely guaranteed from all of them prior to data collection, their privacy was thoroughly secured as the data collected anonymously, only files numbers were registered to avoid data duplication.
Statistical analysis
After being collected, the data was entered to Statistical Package of Social Sciences (SPSS) for windows version 21, which is used for analysis of continuous and categorical variables, extracting summary plots and tables, exploring correlation and association between the studied attributes. Chisquare test and Fisher`s Exact test were employed when relevant considering significance level (P.value) of less than (0.05) for judging statistical importance.
Results
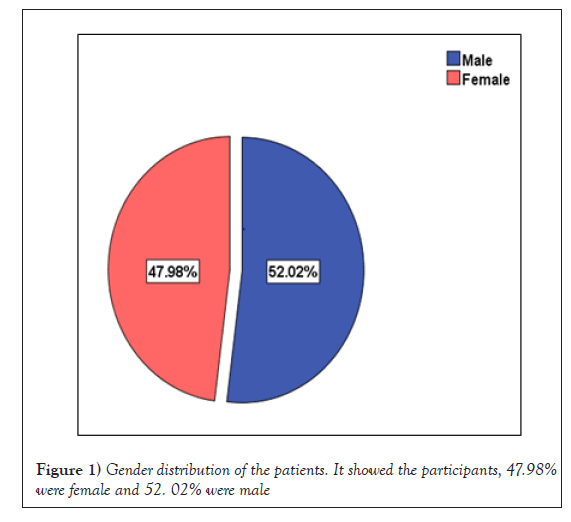
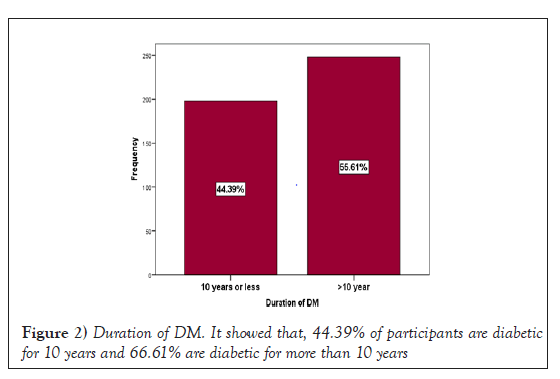
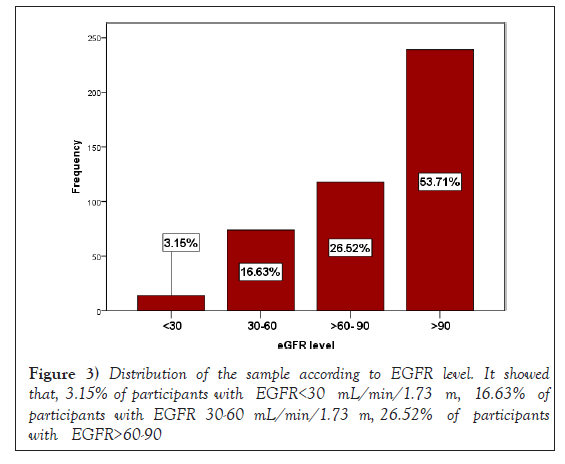
The study included 500 diabetic patients, (52%) are males, and (48%) are females, (Figure 1). Their age ranged from 22-94 years old. Approximately, (55.6%) have diabetes for more 10 years (Figure 2). Around (88.6%) of patients were used metformin with variable doses and frequencies. The use of metformin by the patients has been studied in more details, in term of doses, forms and frequencies and in combination with other hypoglycaemic agents, (Table 1, Table 2 and Table 3). In this paper work, metformin 850 mg twice daily was used by most of the patients (57.85%). Estimated Renal Glomerular Filtration Rate (ERGFR) of the patients was investigated and classified into four groups. According to the severity of renal impairment, (53.7%) of the patients have EGFR>90 mL/min/1.73 m2, (26.5%) of the patients have EGFR 60-90 mL/min/1.73 m2, (16.6%) of the patients have EGFR 30-60 mL/min/1.73 m2, and (3.2 %) of the patients have EGFR<30 mL/min/1.73 m2, (Figure 3).
| Hypoglycaemic drugs | Percentage of the patient using drugs |
|---|---|
| Sulfonyl urea | 87 (19.51%) |
| Insulin injection | 328 (73.54%) |
| Metformin | 394 (88.6%) |
Table 1: Illustrated hypoglycaemic treatment modality used by the patients
| Metformin Dose/Form | Frequency of Metformin/day | Total | |||
|---|---|---|---|---|---|
| Once | Twice | Three times | Stopped | ||
| 500 | 16 | 20 | 1 | 0 | 37 |
| 850 | 81 | 263 | 9 | 0 | 353 |
| Janumet | 6 | 2 | 0 | 0 | 8 |
| Stopped | 0 | 0 | 0 | 46 | 46 |
| Total | 105 | 285 | 10 | 51 | 444 |
Table 2: Showed dose and frequency of metformin
| Combination of hypoglycaemic treatment | Percentage |
|---|---|
| Metformin+Sulfonylurea | 87 |
| Metformin+Insulin | 328 |
| Insulin+Sulfonylurea | 87 |
Table 3: Showed combination of hypoglycaemic treatment
Metformin and EGFR
In this paper work, metformin use was examined across EGFR level. There are (21.42%) of the patients with EGFR<30 mL/min/1.73 m2 used metformin, only 1% of those patient used once daily and 2% used more than once daily. As well as, (70.27%) of the patients had EGFR from 30-60 mL/min/1.73 m2 were on metformin, of this group only 25.67% of those patients used metformin once daily and (44.59%) used metformin twice to three times a day. About (93.22%) of the patients with EGFR>60-90 mL/min/1.73 m2 and used metformin, and (97.90%) of the patients with EGFR greater than 90 mL/min/1.73 m2 and used metformin. This difference is highly significant using Fisher`s Exact test (Fisher`s Exact=97.5, P value<0.001). However, EGFR is a significant factor determining metformin use (Figure 4 and Table 4).
| EGFR in mL/min/1.73 m2 | Age group | Total | |
|---|---|---|---|
| ≤ 60 years | >60 years | ||
| <30 | 9 | 5 | 14 |
| 30-60 | 15 | 59 | 74 |
| >60-90 | 41 | 77 | 118 |
| >90 | 170 | 69 | 239 |
| Total | 235 | 210 | 445 |
Table 4: The level of EGFR according to age group of participants
Age, sex and duration of DM against EGFR
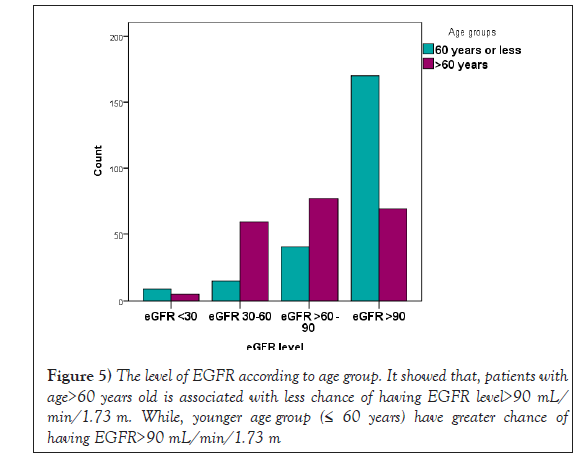
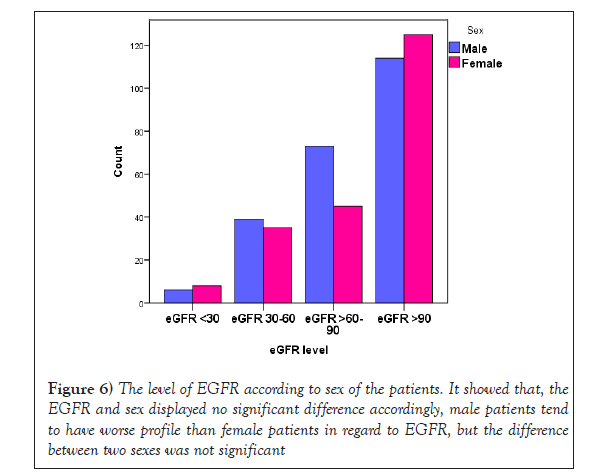
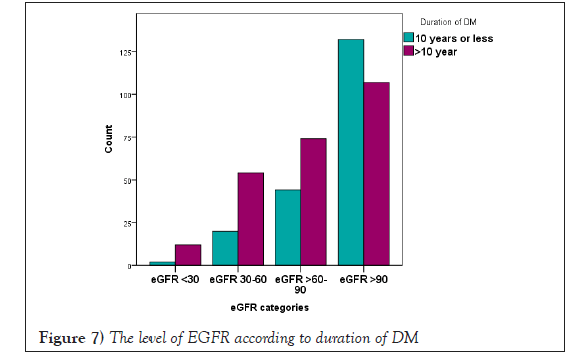
Patients with age>60 years old is associated with less chance of having EGFR level>90. While, younger age groups (≤ 60 years) have greater chance of having EGFR>90 (Table 4 and Figure 5). The difference was highly statistical significant, Pearson Chi-square=79.8, P=0.00. In this paper work, the EGFR and sex showed no significant difference accordingly, male patients tend to have worse profile than female patients in regard to EGFR, but the difference between two sexes was not significant (Table 5 and Figure 6). Duration of DM>10 years is consistently associated with greater probability of having worse EGFR level compared to duration of diabetes mellitus<10 years (Table 6 and Figure 7). The difference was highly significant (Fisher`s Exact=28.2, P=0.00).
| EGFR in mL/min/1.73 m2 | Sex | Total | |
|---|---|---|---|
| Male | Female | ||
| <30 | 6 | 8 | 14 |
| 30-60 | 39 | 35 | 74 |
| >60- 90 | 73 | 45 | 118 |
| >90 | 114 | 125 | 239 |
| Total | 232 | 213 | 445 |
Table 5: The level of EGFR according to sex of the patients
| EGFR in mL/min/1.73 m2 | Duration of DM | Total | |
|---|---|---|---|
| ≤ 10 years | >10 years | ||
| <30 | 2 | 12 | 14 |
| 30-60 | 20 | 54 | 74 |
| >60-90 | 44 | 74 | 118 |
| >90 | 132 | 107 | 239 |
| Total | 198 | 247 | 445 |
Table 6: The level of EGFR according to duration of DM
Baseline characteristics of patients having EGFR between 30-60 mL/ min/1.73 m2
Patients having EGFR of 30-60 mL/min/1.73 m2 were closely inspected in relation to some important variables, they account for (16.59%) of all patients, male to female ratio was very close as it approaches 1.1:1 (39 males:35 females) More than two third of them (59 out of 74) were above 60 years old, Metformin used once a day by (25.67%), twice by (44.59%), however (29.73%) didn’t use metformin. FBS is controlled only in (21.62%) patients; similarly HbA1C which is controlled only in (24.32%), hypertension and ischemic heart disease were Presented in (70.27%) and (22.97%) cases respectively (Table 7).
| Characteristics | Subgroup | No. of patients | Total |
|---|---|---|---|
| Gender | Male | 39 | 74 |
| Female | 35 | ||
| Age | ≤ 60 | 15 | 74 |
| >60 | 59 | ||
| Metformin used by 47 patients | |||
| Dose of Metformin/day | Once | 19 | 74 |
| Twice | 28 | ||
| Three times | 0 | ||
| Not used | 27 | ||
| FBS | Controlled | 16 | 74 |
| High | 58 | ||
| HbA1C | Controlled | 18 | 74 |
| Fair control | 25 | ||
| High | 31 | ||
| Hypertension | Yes | 52 | 74 |
| No | 22 | ||
| IHD | Yes | 17 | 74 |
| No | 57 | ||
Table 7: Baseline characteristics of patients having EGFR 30-60 ml/ min/1.73 m2
TABLE 7
Baseline characteristics of patients having EGFR 30-60 ml/min/1.73 m2
Patients with EGFR<15 mL/min/1.73 m2
There are 4 patients out of 500 with EGFR<15 who are clinically known as End Stage Renal Disease (ESRD), 3 out of 4 are males, 2 out of 4 with age of 60 years old, the other patients` age were between 38 and 47 years old. All of them have diabetes mellitus>10 years. During investigation of FBS and HbA1C, there were 3 patients having high FBS and all 4 patients have poorly controlled HbA1C. Serum creatinine of the 4 patients is elevated and none of them is currently on metformin. There were 3 out of 4 patients are hypertensive and have ischemic heart disease (Table 8).
| Case | Age | Sex | FBS | HbA1C | Duration of DM | S.creat | Metf. use | HPT | IHD | HPT Treat. |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 60 | M | 225 | 9.3 | 23 years | 6 | No | Yes | yes | CCB |
| 2 | 47 | F | 205 | 8.5 | 12 years | 5.2 | No | Yes | Yes | ACEI |
| 3 | 38 | M | 89 | 8 | 22 years | 7 | No | yes | No | CCB |
| 4 | 60 | M | 370 | 9 | 20 years | 6 | No | yes | No | CCB |
Table 8 : Baseline and clinical characteristics of cases with EGFR<15 (ESRD)
Discussion
Type II diabetes is the most common form of diabetes, accounting for around 90% of all diabetic patients. Type II diabetes is most commonly diagnosed in older adults, but is increasingly seen in children, adolescents and younger adults due to rising levels of obesity, physical inactivity and poor diet [16]. It is regarded as the first line treatment for type II diabetes in most guidelines around the world. For forty years metformin has been used to control blood glucose levels in patients with type I diabetes [17]. However, there are several clinical conditions that are considered as contraindications to the use of metformin among patients with type II diabetes mellitus, such as renal dysfunction, CHF, hypersensitivity to metformin, acute or chronic metabolic acidosis, and impaired hepatic function. That is why observation for contraindications of Metformin therapy is essential in type II diabetic patients. In this paper work, 394 out of 446 patients were on metformin therapy. However, (23.99%) had contraindications which necessitate change of metformin regimen or caution. Renal impairment as EGFR<60 mL/ min/1.73 m2 was the most frequently occurring contraindication and was presented in (12.33%) of patients, IHD was the second most common contraindication and was presented in (11.66%) of the patients. Compared with other study that showed CHF is the most common contraindication of metformin [18]. In another study, metformin has been prescribed for patients who are listed in the guidelines as having standard contraindications to its use. There were (28%) patients with impaired renal function (Clcr<60ml/ min) and 4% with Clcr<30ml/min. Moreover, (28%) had IHD, (5%) patients were diagnosed as having CHF, (4%) with chronic obstruction pulmonary disease, and (2%) with peripheral vascular disease [18]. previous studies showed similar prevalence rate of contraindications of metformin, approximately, 89% patients treated with metformin and admitted to a British university Diabetes Clinic, 54% had contraindications or risks precluding metformin treatment [19]. Another study in Germany found that 64% of the studied population had contraindications/precautions to metformin therapy [20]. Another study found that 24.5% of patients prescribed metformin have contraindications to its use [21].
Metformin and Estimated Glomerular Filtration Rate (EGFR)
The best test to measure the level of kidney function and to determine the stage of kidney disease is EGFR. According to the National Kidney Foundation, normal results range from 90 to 120 mL/min/1.73 m2. Older people will have lower than normal GFR levels, because GFR decreases with age. In adults, the normal EGFR number is more than 90 and it declines with age, even in people without kidney disease [22]. Metformin is one of the oldest and most widely prescribed antidiabetic drugs worldwide. It is the only such medicine that has shown a reduction of cardiovascular mortality in type II diabetes mellitus. Metformin’s costs are lower, and in many underdeveloped countries this is the only medicine available for poor patients. It causes a reduction in mortality by decreasing cardiovascular complications [6]. In April 2016; the FDA reviewed their warning with regards to metformin use in patients with impaired kidney function, defining the renal impairment according to EGFR. The reviewed guidelines stated that the use of metformin is only absolutely contraindicated in patients with severe CKD (EGFR<30 ml/min/1.73 m2). Therefore, patients with moderate CKD (EGFR 30-59 ml/min/1.73 m2) are eligible to receive metformin. A previous study reported that the use of metformin in patients with type II diabetes mellitus and advanced CKD was associated with a significantly increased risk of all-cause mortality compared with non-users [23]. This raises the concern that a decline in renal function in patients with moderate CKD receiving metformin may increase the risk of toxicity to metformin. There is high prevalence of CKD in diabetic patients and there is no agreement among physicians regarding the risk of Metformin Associated Lactic Acidosis (MALA) in diabetic patients with CKD. In this paper work we identified the prescription pattern of metformin across CKD stages in diabetic participants. Patient with EGFR<30 mL/min/1.73 m2 and still using metformin, impairments were severe enough to avoid metformin use. The patients with EGFR from 30-60 mL/min/1.73 m2 used metformin were above 60 years of age and with non-controlled FBS and HbA1C, hypertension and ischemic heart disease. Therefore, renal function should be monitored closely in type II diabetic patients using metformin. Monitoring is important every 6 month, as up to 90% of renal function can be lost before clinical symptoms of renal failure become apparent [24]. University of Chicago diabetes center reported that, 15.3% patients with EGFR of<60ml ml/min/1.73m2 were receiving metformin [25]. Salpeter et al. 2010 found that diabetic patients using metformin with GFR levels between 30-60 mL/min/1.73 m2, lactic acidosis is still exceedingly rare even in the presence of comorbid conditions. One study found that the clearance of metformin decreases by about 75% when the EGFR is <60 mL/min/1.73 m2 without further change when the EGFR declines to 30 mL/min/ 1.73 m2; however, serum concentrations of metformin at both EGFR levels are only about two-fold higher than in normal kidney function [26]. Observational study made by the Reduction of Atherothrombosis for Continued Health (REACH) illustrated that>19,000 subjects with history of atherothrombotic disease, 1,572 patients were using metformin with EGFR 30-60 ml/min/1.73m2, found that metformin was associated with 24% reduction in all-cause mortality. Therefore, there is no correlation or any known relationship between renal function, metformin levels and MALA [25]. In this paper work, Most of patients was take metformin 850 mg twice a day and some of them have ischemic heart disease their EGFR<60 mL/ min/1.73 m2. The result of our study found that patients on frequent doses of metformin are more liable to get lactic acidosis which is supported by a previous study that showed a significant correlation between the lactate levels and the metformin dose [26]. This study found that the metformin use was common in diabetics with EGFR from 30-60 mL/min/1.73 m2 and rarely prescribed in patients with EGFR<30 mL/min/1.73 m2. Therefore, the contraindications were significantly less frequent in those started on metformin compared to those who were not. It was not known if this was due to prescribers’ awareness of the contraindications of metformin in diabetic patients. In the United States, metformin is still commonly prescribed for diabetic patients with mild to moderate CKD. The revised guidelines stated that the use of metformin is only absolutely contraindicated in patients with severe chronic kidney disease (CKD) (EGFR<30 ml/min/1.73 m2). Therefore, patients with moderate CKD (EGFR 30-59 ml/min/1.73 m2) are eligible to receive metformin. Collins et al, reported that the use of metformin in patients with type II diabetes mellitus and advanced CKD was associated with a significantly increased risk of all-cause mortality compared with non-users. This advances the concern that a decline in renal function in patients with moderate CKD receiving metformin may increase the risk of toxicity to metformin. Metformin is primarily excreted unchanged by the kidney, and renal impairment may cause the accumulation of metformin leading to an elevated metformin concentration, and this has been proposed to lead to lactic acidosis [27]. In our study most patients were 60 years or less (52.7%) and the calculation of EGFR level was made according to age groups and illustrated that younger age group (≤ 60 years) have less chance of having very low EGFR (<30 mL/min/1.73 m2), and greater chance of having EGFR>90. The result supported by Takenouchi et al, 2015 found that GFR declines by about 10 mL/min every 10 years after the age of forty. However, another study, have shown that metformin does not raise lactate levels even an elderly and in those with reduced renal function [28].
Metformin and impaired renal function
Impaired renal function can lead to the accumulation of metformin, and elevated concentrations of metformin have been associated with lactic acidosis. The use of metformin is contraindicated in men and women with serum creatinine concentrations of 1.5 mg/dL or higher and 1.4 mg/dL or higher, respectively, due to the risk of the life-threatening complication, lactic acidosis [29]. Abnormal kidney function remains the biggest contraindication for metformin until early 2016, US FDA guidelines reversed its use with a serum Creatinine (Cr)>132.63 mmol/L (1.5 mg/dL) in men and>123.79 mmol/L (1.4 mg/dL) in women [30]. Lalau et al, 2015 compared a group of patients receiving 850 mg metformin daily with (CrCl) of 30-60 mL/min with another group that received 1700 mg of metformin daily with CrCl>60 mL/min. There was no significant difference in serum levels of metformin and lactate between the two groups [31]. In another study of a group of patients with CrCl 15-40 mL/min, found that no correlation was found between lactate and metformin levels, and the patients were even on dialysis [32]. However, in this study, serum creatinine level was estimated according to patient’s sex. Most of the patients (46.9% male and 43.5% female) have normal creatinine level. Accordingly, serum Cr measurements are not an accurate reflection of the GFRs and it’s not an absolute contraindication for metformin use in diabetic patient with renal disease. Therefore, renal impairment should be detected according to EGFR and measurement of serum creatinine alone is not a reliable indicator of renal function and should not be used in isolation for the purpose of prescribing medicines safely
Glycated haemoglobin and renal function
In this paper work, HbA1c was only 22.41% of the patients have good glycemic control. In the U.K. Prospective Diabetes Study (UKPDS), the largest previously reported randomized trial of glycemic control in patients with type II diabetes, tighter glucose control did not reduce the incidence of major renal outcomes, although there was some evidence of a reduction in the development of microalbuminuria and obvious proteinuria with a prolonged follow-up period [33-35]. Consistency of glycemic control is important to preserve kidney function in type II diabetic patients, in particular, in those with nephropathy [34,36-42].
Conclusion
Other contraindications that was not present in this paper work including hepatic disease and chronic obstructive pulmonary disease. During the research there was no patient having either one of them. However, the US Food and Drug Administration FDA have removed heart failure as a contraindication for metformin use in 2006, since reduction in all-cause mortality with metformin use was demonstrated in diabetics with heart failure. Another study, illustrated that diabetic patients with pulmonary disease is another contraindication for metformin use. Conditions that can result in increased lactate production or decreased lactate elimination have therefore been emphasized. Lactate production is increased as a result of severe tissue hypoxia such as IHD. In this study were 13.7% patients have IHD, most of them are above 60 years old on metformin and their profiles were unsatisfactory and uncontrolled, accordingly, those patients have more incidents to cardiac failure. Other study found that, age, IHD and poorer glycemic control are predictors of the development of cardiac failure. Salpeter et al, 2010 conducted a Cochrane review, there were 347 prospective trials and cohort studies were included with more than 70490 patients who were using metformin. They found that at least one contraindication was present in 97% of the studies. Metformin was not associated with increased risk of LA compared with other antidiabetic medicines; instead, comorbidities causing tissue hypoxia were the main risks for LA. In this paper work, cardiac medications commonly prescribed such as Angiotensin Converting Enzyme-Inhibitors (ACE-I) with metformin. Combination of ACEI and metformin has been reported to have a possible synergistic effect on the development of hyperkalaemic lactic acidosis. Although, there are multi-risk factors associated with metformin induced lactic acidosis including severe dehydration (i.e., reduced tissue perfusion), CHF, sepsis, shock, hypoxia, hepatic impairment, advanced age, and excessive alcohol intake may also increase the risk of metformin-associated lactic acidosis. Nonetheless, use of metformin in type II diabetes mellitus makes management of blood sugars somewhat simpler as it has been shown that the incidence of hypoglycaemia from oral hypoglycaemic like glibenclamide was significantly greater than that of LA. There are several considerations we have to know:
• Metformin is frequently most drug used in Libyan patients.
• The prevalence of metformin contraindication was 23.99%.
• The most frequent contraindication in this paper work was CKD and IHD due to it is risk factor for CHF was the second one.
• Physicians rely on serum creatinine, as an indicator for renal function; they should investigate EGFR as an indicator.
• None of the patients was treated according to National kidney Foundation guidelines because; guidelines are disregarded by the physicians in clinical practice in Libya.
• Lack of clinical pharmacists serving in Benghazi diabetic clinic in Libya which is another factor increasing the risk of such oversights.
• Since age and poor control are risk for CKD. It is essential that prescribers develop a better understanding of the prescribing guidelines for metformin and its adverse effect on renal function in patients with type II diabetes mellitus and moderate CKD.
Recommendations
• The risk of lactic acidosis increases with the degree of renal dysfunction and the patient’s age. So, we advise all the Physicians for measurement of Creatinine Clearance (CrCl) for patients that initiated metformin therapy.
• We are also recommending that the measure of kidney function changed from blood creatinine concentration to GFR estimating equation (EGFR), Because GFR decline to approximately half the normal level before serum creatinine concentration rises above the upper limit of normal.
• It is essential that prescribers develop a better understanding of the prescribing guidelines for metformin and its adverse effect on renal function in patients with type II diabetes mellitus, old age, moderate CKD.
• With close follow up of renal function in those patients.
REFERENCES
- Malerbi DA, Franco LJ. Multicenter study of the prevalence of diabetes mellitus and impaired glucose tolerance in the urban Brazilian population aged 30–69 yr. Diabetes Care. 1992;15(11):1509-16.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(1):S81-S90.
- Al-Goblan AS, Al-Alfi MA, Khan MZ. Mechanism linking diabetes mellitus and obesity. Diabetes Metab Syndr Obes. 2014;7:587-91.
- Knol MJ, Twisk JW, Beekman AT, et al. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49(5):837-45.
- Inzucchi SE, Sherwin RS (2011) Type 2 diabetes mellitus: Cecil Medicine. (24th edn), Philadelphia, Pa: Saunders Elsevier. e78-e94.
- Alberti KGMM, Zimmet P, Shaw J. International Diabetes Federation: a consensus on Type 2 diabetes prevention. Diabet Med. 2007;24(5):451-63.
- Hsu WH, Hsiao PJ, Lin PC, et al. Effect of metformin on kidney function in patients with type 2 diabetes mellitus and moderate chronic kidney disease. Oncotarget. 2018;9(4):5416.
- Rena G, Hardie DG, Pearson E. The mechanisms of action of metformin. Diabetologia. 2017;60(9):1577-85.
- Marshall SM. 60 years of metformin use: A glance at the past and a look to the future. 2017;1561-65.
- Bridges HR, Jones AJ, Pollak MN, et al. Effects of metformin and other biguanides on oxidative phosphorylation in mitochondria. J Biochem. 2014;462(3):475-87.
- Eppenga WL, Lalmohamed A, Geerts AF, et al. Risk of lactic acidosis or elevated lactate concentrations in metformin users with renal impairment: a population-based cohort study. Diabetes Care. 2014;37(8):2218-24.
- Panchapakesan U, Pollock C. Drug repurposing in kidney disease. Kidney international. 2018;94(1):40-48.
- Corremans R, Vervaet BA, D’Haese PC, et al. Metformin: A Candidate Drug for Renal Diseases. Int J Mol Sci. 2019;20(1):42-57.
- Viollet B, Guigas B, Garcia NS, et al. Cellular and molecular mechanisms of metformin: An overview. Clinical Science. 2012;122(6):253-70.
- Lalau JD, Kajbaf F, Bennis Y, et al. Metformin treatment in patients with type 2 diabetes and chronic kidney disease stages 3A, 3B, or 4. Diabetes Care. 2018;41(3):547-53.
- World Health Organization. Definition and diagnosis of diabetes mellitus and intermediate hyperglycaemia: Report of a WHO/IDF consultation. 2006.
- Graham GG, Punt J, Arora M, et al. Clinical pharmacokinetics of metformin. Clin Pharmacokinet. 2011;50(2):81-98.
- Sweileh WM. Contraindications to metformin therapy among patients with type 2 diabetes mellitus. Pharmacy World and Science. 2007;29(6):587-92.
- Al Awadhi SS, Clifford RM, Sunderland VB, et al. Do contraindications to metformin therapy deprive type 2 diabetic patients of its benefits. Int J Diabetes Metabol. 2008;16:81-84.
- Sulkin TV, Bosman D, Krentz AJ. Contraindications to metformin therapy in patients with NIDDM. Diabetes Care. 1997;20(6):925-28.
- Hauner H. Verbreitung des Diabetes mellitus in Deutschland. Wien Klin Wochenschr. 1998;123(24):777-82.
- Emslie‐Smith AM, Boyle DI, Evans JMM, et al. Contraindications to metformin therapy in patients with Type 2 diabetes-a population‐based study of adherence to prescribing guidelines. Diabet Med. 2001;18(6):483-88.
- Coresh J, Astor BC, Greene T, et al. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am J Kidney Dis. 2003;41(1):1-12.
- Hung SC, Chang YK, Liu JS, et al. Metformin use and mortality in patients with advanced chronic kidney disease: National, retrospective, observational, cohort study. Lancet Diabetes Endocrinol. 2015;3(8):605-14.
- Hirani V, Naganathan V, Blyth F, et al. Multiple but not traditional risk factors predict mortality in older people: The Concord Health and Ageing in Men Project. Age. 2014;36(6):9732.
- Frid A, Sterner GN, Londahl M, et al. Novel assay of metformin levels in patients with type 2 diabetes and varying levels of renal function: clinical recommendations. Diabetes Care. 2010;33(6):1291-93.
- Collins AJ, Foley RN, Chavers B, et al. US renal data system 2011 annual data report. Am J Kidney Dis. 2012;59(1):A7.
- Bipi PK, George J, Gomathy S, et al. Lactate levels and risk of lactic acidosis with metformin in diabetic kidney disease patients. Saudi J Kidney Dis Transpl. 2017;28(6):1356-61.
- Heaf JG, Van Biesen W. Metformin and chronic renal impairment: A story of choices and ugly ducklings. Clinical Diabetes. 2011;29(3):97- 101.
- Lipska KJ, Bailey CJ, Inzucchi SE. Use of metformin in the setting of mild-to-moderate renal insufficiency. Diabetes Care. 2011;34(6):1431-37.
- Foundation NK. KDOQI clinical practice guideline for diabetes and CKD: 2012 update. Am J Kidney Dis. 2012;60(5):850-86.
- LalauJD, Vermersh A, Hary Letal. Type 2 diabetes in the elderly: an assessment of metformin (metformin in the elderly). Int J Clin Pharmacol Ther Toxicol. 1990;28:329-32.
- Lalau JD, Arnouts P, Sharif A, et al. Metformin and other antidiabetic agents in renal failure patients. Kidney Int. 2015;87(2):308-22.
- ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. New England J Med. 2008;358(24):2560-72.
- Brownlee M. The pathobiology of diabetic complications: a unifying mechanism. Diabetes. 2005;54(6):1615-25.
- Radcliffe NJ, Seah JM, Clarke M, et al. Clinical predictive factors in diabetic kidney disease progression. J Diabetes Investig. 2017;8(1):6-18.
- Takenouchi A, Tsuboi A, Terazawa-Watanabe M, et al. Direct association of visit-to-visit HbA1c variation with annual decline in estimated glomerular filtration rate in patients with type 2 diabetes. J Diabetes Metab Disord. 2015;14(1):69.
- Sulkin TV, Bosman D, Krentz AJ. Contraindications to metformin therapy in patients with NIDDM. Diabetes Care. 1997;20(6):925-8.
- Nichols GA, Gullion CM, Koro CE, et al. The incidence of congestive heart failure in type 2 diabetes: an update. Diabetes Care. 2004;27(8):1879-84.
- Malmberg K. DIGAMI. Diabetes Mellitus, Insulin Glucose Infusion in Acute Myocardial Infarction Study Group. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314(7093):1512-15.
- Salpeter SR, Greyber E, Pasternak GA, et al. Risk of fatal and nonfatal lactic acidosis with metformin use in type 2 diabetes mellitus. Cochrane Database Syst Rev. 2010;(4):1-12.
- Franzetti I, Paolo D, Marco G, et al. Possible synergistic effect of metformin and enalapril on the development of hyperkaliemic lactic acidosis. Diabetes Res Clin Pract. 1997;38(3):173-6.