Use of methylene blue in hepatic arterial infusion pump resulting in serotonin syndrome. A case report
Received: 02-Feb-2018 Accepted Date: Feb 21, 2018; Published: 26-Feb-2018
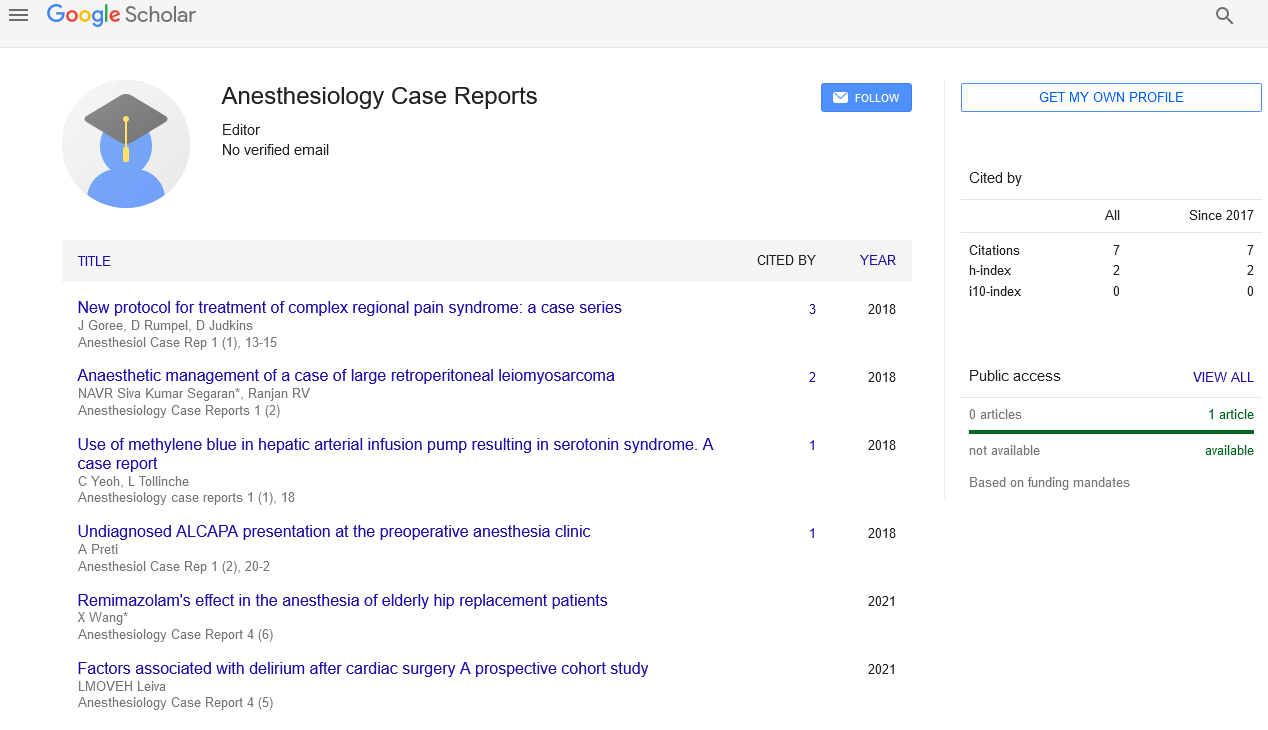
Citation: Yeoh C, Tollinche L. Use of methylene blue in hepatic arterial infusion pump resulting in serotonin syndrome. A case report. Anesthesiol Case Rep. 2018;1(1):18-19.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
We report a case of a 35 year old woman with colon cancer metastatic to liver and lung who presented for exploratory laparotomy and/placement of hepatic arterial infusion pump for chemotherapy. Surgical course was notable for aberrant hepatic artery anatomy requiring extended dissection time, vascular surgery consultation, and use of substantial methylene blue to aid in visualization. Of note, patient’s history was also significant for anxiety and depression, for which she was being treated with the selective serotonin reuptake inhibitor (SSRI) duloxetine (Cymbalta). The patient subsequently developed serotonin syndrome in the postoperative period but fully recovered. Our case highlights the need for close attention to methylene dosing recommendations and improved communication between perioperative care providers (surgery, anesthesia, nursing, and pharmacy) to prevent such occurrences.
Keywords
Serotonin syndrome; Methylene blue
Introduction
Methylene blue is a phenothiazine derivative commonly used in medicine for staining and therapeutic purposes. It is a potent monoamine oxidase (MAO) inhibitor but is considered a relatively safe drug with few adverse effects and is often used during surgical procedures to assist with identification of structures such as nerves, tissues, and endocrine glands [1]. Methylene blue also has therapeutic indication in the treatment of methemoglobinemia, vasoplegic shock, Alzheimer’s disease, and pediatric Malaria [2]. Dosing regimen varies depending on indication for use and route of administration [2].
The most common side effect of methylene blue is an abnormal urine or stool color. Less common side effects include but are not limited to mild bladder irritation, frequent urination, dizziness, nausea and vomiting, abdominal pain, diarrhea, headaches, and increased sweating (rxlist.com). An uncommon, albeit potentially catastrophic, side effect of methylene blue administration is serotonin syndrome. Administration of methylene blue on its own however, has not been known to cause serotonin toxicity [3].
Serotonin syndrome, precipitated by concurrent use of methylene blue and SSRIs, is characterized by a triad of mental status, autonomic, and neuromuscular clinical signs and symptoms [4]. In the presence of a serotonergic agent, serotonin syndrome can be confirmed with high probability by the presence of one of five conditions described by Hunter’s Serotonin Toxicity Criteria (Table 1) [3].
| 1 | Spontaneous clonus |
| 2 | Tremor AND hyperreflexia |
| 3 | Inducible clonus AND agitation OR diaphoresis |
| 4 | Ocular clonus AND agitation OR diaphoresis |
| 5 | Hypertonicity AND temperature >38ºC AND Inducible clonus OR ocular clonus |
Table 1: Hunter Serotonin Toxicity Criteria (Table adapted from Locke A, Methylene Blue and the Risk of Serotonin Toxicity, June 2015 [3]).
Case Report
A 35 year old female with past medical history significant for anxiety, hypertension, and colorectal carcinoma presented for exploratory laparotomy and placement hepatic arterial infusion pump for treatment of disease recurrence with metastases to liver and lung. Because of aberrant hepatic vasculature requiring extended dissection time and intraoperative vascular surgery consultation, the total operating time was a protracted 8 h. Methylene blue was injected by the surgeon directly into the liver to delineate hepatic vasculature and help in confirming hepatic pump placement. A total of 85 mL of 0.5% methylene blue was administered by the surgeon. Methylene blue vials were ordered and dispensed from pharmacy with dose recommendation of up to 7 mg/Kg or 560 mg (112 mL of 0.5% methylene blue) [5]. The surgeon documented that patient was receiving SSRI preoperatively, but it is unclear if surgeon was aware of the dangers of concomitant administration of methylene blue and SSRI. In addition, fentanyl was administered intraoperatively, and serotonin toxicity has also been described with concurrent use of MAO-inhibitors and phenylpiperidine series opioids [6,7]. Because the patient had also been on SSRIs and received an extremely high dose of methylene blue during surgery, she was monitored closely in the PACU postoperatively for symptoms of serotonin syndrome. While her recovery was initially uneventful, on postop day 1, she became increasingly lethargic with tachypnea, tachycardia, hyperreflexia, and myoclonus was elicited. Due to the severity and progression of symptoms, care was escalated and the patient was evaluated by the critical care service and psychiatry. Cyproheptadine was started and all serotonergic agents were discontinued. While a rare occurrence, cyproheptadine causing hepatitis and acute liver failure has been reported [8]. Hence, liver function tests were monitored during her treatment with cyproheptadine. The patient’s symptoms improved over the next couple of days and she was restarted on SSRI and discharged home uneventfully on postoperative day 7.
Discussion
While there are multiple indications for the use of methylene blue in medicine, its use in vascular surgery for visualization are not well-described. Our case describes the injection of methylene blue directly into a hepatic arterial infusion pump to assist with confirmation of vasculature during pump placement. Due to aberrant anatomy, multiple doses of methylene blue were required over the course of surgery, with the cumulative dosage nearing maximum dose recommendations for the drug (7 mg/Kg in the treatment of methemoglobinemia) [5].
Dosing guidelines for methylene blue from various sources generally recommend 1-2 mg/Kg intravenously [9]. Unfortunately, given the multiple medical indications for methylene blue, dosing regimens also vary widely based on clinical indication (Table 2) [2]. This variability in dose recommendations can also cause confusion and result in inaccurate dosing if clinical indications are not clearly defined.
| Therapeutic indication | Dosage of Methylene Blue |
| Inherited methemoglobinemia | 1 × 50-250 mg/day (for a lifetime) [10] |
| Acute methemoglobinemia | 1-2 × 1.3 mg/Kg (i.v. over 20 min) |
| Ifosfamid-induced neurotoxicity | 4 × 50 mg/day p.o. or i.v. [11] |
| Prevention of urinary tract infections in elderly patients | Orally 3 × 65 mg/day |
| Vasoplegic adrenaline-resistant shock | 200 mg i.v. over 1 h followed by infusion (0.25-2 mg/Kg/h) [12] |
| Alzheimer's disease | 3 × 60 mg/day [13] |
| Pediatric malaria | 2 × 12 mg/Kg p.o. for 3 days |
Table 2: Methylene Blue dosage in different clinical conditions (Table adapted from Schirmer et al , 2011 [2]).
Postoperatively, the patient was monitored closely for symptoms of serotonin toxicity. Due to the high index of suspicion, the patient was managed and treated appropriately at the first signs of the syndrome. Treatment of serotonin syndrome includes discontinuation of all serotonergic agents, support of vitals, benzodiazepines for sedation, and cooling therapy for hyperthermia [14]. Serotonin receptor antagonists such as cyproheptadine, chlorpromazine, olanzapine, and ketanserin may be used for moderate or severe cases [13,14].
In a systematic review by Bradley Ng et al. in 2010, nine case reports and two retrospective reviews on methylene blue and serotonin syndrome were identified. Twenty-six patients were reported to have acute confusional state suggestive of serotonin syndrome after methylene blue administration. Of these patients, 24 were on SSRIs and 1 patient was on clomipramine. Serotonin syndrome was a possible diagnosis in all 25 patients [15]. Despite this known association, concomitant SSRI administration is not a contraindication to methylene blue administration. Instead, recommendations suggest a cautious risk/benefit analysis in determining need for methylene blue. Experts urge clinicians to consider an alternative agent to methylene blue in this setting. Importantly, providers must be aware of the possible interaction of methylene blue with SSRIs. Education efforts should continue to this end and in the event of concomitant administration, vigilance must be ensured for signs/ symptoms of serotonin syndrome.
Conclusion
Our case highlights the need for improved communication between all services involved in the intraoperative care of a patient (surgery, anesthesia, OR nursing, pharmacy) [16]. This is of utmost importance especially when cases are complicated requiring interventions that deviate from routine practice. Good communication allows for better coordination of care and serves to prevent events that can otherwise cause harm if allowed to reach the patient.
Methylene blue is a relatively safe drug with multiple indications [17]. Because the indications and modes of use vary widely, it is imperative that dosing recommendations are clearly defined for specific indications. As applies to the use of all drugs, it is also crucial that healthcare providers familiarize themselves with indications, adverse effects, interactions, and dose recommendations so as to avoid medication errors that can potentially cause serious patient harm.
Acknowledgement
The authors’ work was supported and funded in part by NIH/NCI Cancer Center Support Grant P30 CA008748
REFERENCES
- Francescangeli J, Vaida S, Bonavia AS. Perioperative Diagnosis and Treatment of Serotonin Syndrome Following Administration of Methylene Blue. Am J Case Rep 2016;17:347-51.
- Schirmer RH, Adler H, Pickhardt M, et al. “Lest we forget you — methylene blue …”. Neurobiol Aging 2011;32(12):2325.
- Locke A. Methylene Blue and the Risk of Serotonin Toxicity. J Anesthesia Patient Safety Foundation, June 2015.
- Rowley M, Riutort K, Shapiro D, et al. Methylene Blue-Associated Serotonin Syndrome: A ‘Green’ Encephalopathy After Parathyroidectomy. Neurocrit Care 2009;11(1):88-93.
- Methylene Blue Drugs A to Z. 2016.
- Larson KJ, Wittwer ED, Nicholson WT, et al. Myoclonus in patient on fluoxetine after receiving fentanyl and low-dose methylene blue during sentinel lymph node biopsy. J Clin Anesth ;27(3):247-51.
- Gillman PK. Monoamine oxidase inhibitors, opioid analgesics and serotonin toxicity. BJA 2005;95(4):434-41.
- Chertoff J, Alam S, Clark V. Cyproheptadine-Induced Acute Liver Failure. ACG Case Rep J 2014;1(14):212-3.
- Methylene Blue. online.lexi.com: Lexicomp 2018.
- Cawein M, Behlen CH, Lappat EJ, et al. Hereditary diaphorase deficiency and methemoglobinemia. Arch Intern Med 1964;113:578-85.
- Pelgrims J, De Vos F, Van den Brande J, et al. Methylene blue in the treatment and prevention of ifosfamide-induced encephalopathy: report of 12 cases and a review of the literature. Br J Cancer 2000;82(2):291-4.
- Warth A, Goeppert B, Bopp C, et al. Turquoise to dark green organs at autopsy. Virchows Arch 2009;454(3):341-4.
- Wischik CM, Bentham P, Wischik DJ, et al. Tau aggregation inhibitor (TAI) therapy with remberTM arrests disease progression in mild and moderate Alzheimer's disease over 50 weeks. Alzheimer's & Dementia: J Alzheimer's Assoc 2008;4(4):T167.
- Frank C. Recognition and treatment of serotonin syndrome. Can Fam Physician 2008;54(7):988-92.
- Ng BK, Cameron AJ. The Role of Methylene Blue in Serotonin Syndrome: A Systematic Review. Psychosomatics 2010;51(3):194-200.
- Arora V, Johnson J, Lovinger D, et al. Communication failures in patient sign-out and suggestions for improvement: a critical incident analysis. Qual Saf Health Care 2005;14(6):401-7.
- Ginimuge PR, Jyothi SD. Methylene Blue: Revisited. J Anaesthesiol Clin Pharmacol 2010;26(4):517-20.