Are the pharmaceutical or alternative treatments most effective to treat Alzheimer's disease?
Received: 06-Sep-2023, Manuscript No. PULJNCN-23-6697; Editor assigned: 08-Sep-2023, Pre QC No. PULJNCN-23-6697 (PQ); Reviewed: 22-Sep-2023 QC No. PULJNCN-23-6697; Revised: 23-Jan-2024, Manuscript No. PULJNCN-23-6697 (R); Published: 30-Jan-2024
Citation: Boyer B. Are the pharmaceutical or alternative treatments most effective to treat Alzheimer's disease?. J Neurol Clin Neurosci. 2024;8(1):1-5.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Alzheimer's Diseases (AD) is the most prevalent cause of dementia, affecting over 850,000 individuals in the UK alone. The disease is characterized by cognitive decline and significant impairment in daily functioning, driven primarily by the accumulation of amyloid and tau proteins in the brain. Current pharmaceutical treatments for AD include Donepezil, a cholinesterase inhibitor, and Memantine, an N-methyl-D-aspartate receptor antagonist. These drugs aim to manage symptoms by modulating neurotransmitter activity and receptor function. Despite some success, these treatments often show limited efficacy and are not universally effective across all stages of AD.
Alternative therapies, such as music therapy, coenzyme Q10 supplementation, and electroacupuncture, are also being explored. Music therapy has shown promise in improving cognitive and psychiatric symptoms in AD patients, though evidence is limited and often qualitative. Coenzyme Q10, an antioxidant, may reduce oxidative stress and mitochondrial dysfunction, potentially mitigating AD symptoms. Electroacupuncture has demonstrated effects in reducing neurodegeneration in animal models but lacks extensive human trial data. A critical evaluation of these treatment approaches reveals that pharmaceutical methods generally offer more robust evidence of efficacy, particularly in clinical settings. Randomized Controlled Trials (RCTs) of Donepezil and Memantine provide clearer indications of their benefits and limitations compared to the more varied and less quantifiable results from alternative therapies. Despite the potential of alternative treatments, their current evidence base is less compelling, often due to smaller sample sizes, lack of standardization, and limited human trial data.
In conclusion, while alternative therapies present interesting possibilities and may complement traditional treatments, pharmaceuticals remain the primary method for managing Alzheimer's disease. Further research into alternative methods is needed to establish their efficacy and integrate them effectively into comprehensive AD care strategies.
Keywords
Alzheimer's diseases; Pharmaceutical treatments; Alternative therapies; Neurodegeneration
Introduction
According to NHS UK, Alzheimer's disease is the most common cause of dementia in the UK. Dementia is an acquired loss of cognition in multiple cognitive domains sufficiently severe to affect social or occupational function [1].
Research conducted shows over 850,000 people in the UK are living with dementia and around 6 in 10 dementia sufferers in the UK have Alzheimer’s. The risk of Alzheimer's disease and other types of dementia increases with age, affecting an estimated 1 in 14 people over the age of 65 and 1 in every 6 people over the age of 80. Alzheimer’s is caused by a build up of two proteins, called amyloid and tau causing an increasing number of brain cells to become damaged, leading to the symptoms of Alzheimer’s. Symptoms include apathy, dysphoria, memory lapses, aphasia, and a lack of visuospatial awareness. Research submitted to the BMJ suggests, dementia costs to UK health and social services were estimated at £11.6bn in 2012 [2-4].
Literature Review
Pharmacology of current favoured pharmaceutical treatment methods
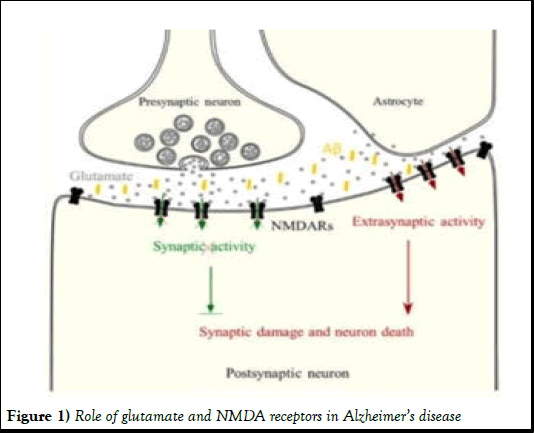
When treating Alzheimer’s Disease (AD), the most commonly prescribed drug in Mild-to moderate Alzheimer’s sufferers is Donepezil-a cholinesterase inhibitor. According to Alzheimer’s research UK, cholinesterase inhibitors increase levels of acetylcholine in the brain which helps allow synaptic transmission in the brain [5]. The most common drug for moderate-to severe Alzheimer’s is Memantine an N-Methyl-D-Aspartate Receptor (NMDAR) antagonist. Regarding, the author states that in AD patients, glutamate released from astrocytes activates extrasynaptic NMDARs and triggers pro-apoptotic signaling (red) that overcomes synaptic NMDAR mediated survival signaling (green) (Figure 1).
Figure 1) Role of glutamate and NMDA receptors in Alzheimer’s disease
Memantine preferentially blocks NMDA receptor activity when the channel is excessively open [6]. The blocking of these NMDARs reduces the effects of Alzheimer’s by preventing pro-apoptotic pathway activation and prolonging brain functionality.
Critical evaluation of pharmaceutical and alternative methods to treating ad
A study concluded Donepezil shows moderate evidence of improvement in cognitive function and completion of daily activities in various stages of the 8257 AD patients in the study. The article aforementioned contained sufficient data from 28 studies of double-blind randomized controlled trials. This trial method is the gold standard for the removal of bias which gives more confidence in the credibility of the data. On the contrary, the information provided in the results states that, of these 28 studies, 17 studies were funded by sponsorships or industry-funded, 4 independently, and 9 with no information on the source of funding. The lack of available tracing of the source of funding for the 9 studies with undisclosed benefactors reduces the strength of the data as the funding of those specific trial locations could potentially have an underlying bias involved.
Data accumulated by Birks and Harvey is corroborated by Birks confirming an improvement in cognitive function when using donepezil in various stages of AD. Both studies boast a clear positive correlation between taking Donepezil at the recommended dose and improved cognition in Alzheimer’s patients however, the latter study is more than 15 years old which makes it an outdated source. The data is also qualitative making it difficult to objectively compare with other studies. The study was conducted as a blind, randomised trial which minimises allocation and selection biases but the potential for assessment bias is present as the trial was not double blind. To ensure integrity and reliability in the results, the trial would need to be double-blind to further reduce any possible bias associated with the trial coordinator. Finally, the data collated unfortunately does not look at the effects of Donepezil individually but rather 3 different types of cholinesterase inhibitors, therefore, the results are reliable but, they are unfortunately not valid as the results obtained do not address the specific effects of donepezil meaning we cannot identify the efficacy of donepezil for reducing AD symptoms [7].
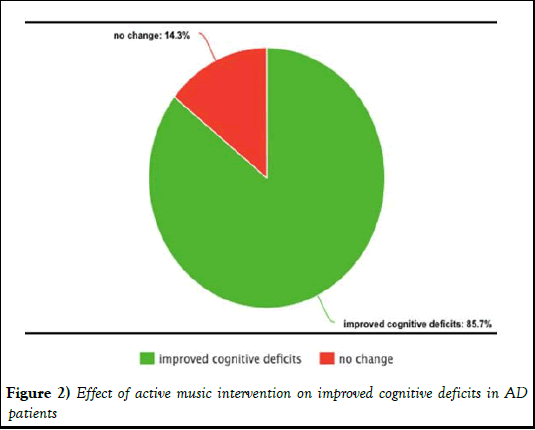
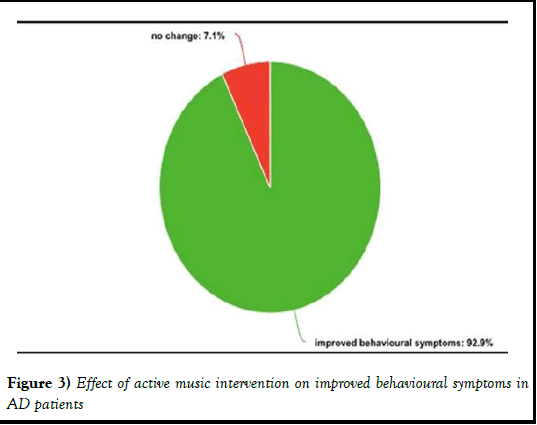
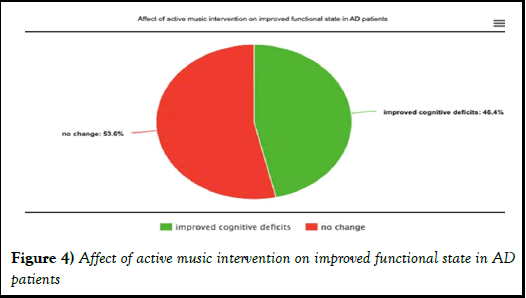
An extensively researched alternative therapy is musical therapy. Stratified analysis found musical therapy enhanced memory and language ability in mild AD patients as well as reduced psychiatric symptoms and caregiver distress in moderate and severe AD patients [8]. This study was a Randomised Control Trial (RCT) which ensures clinical equipoise as it reduces any ethical bias related to the results of the study by assuming that any single specific intervention is better than another. Conversely, it requires a large sample size with study groups across multiple sites to ensure the validity of the results. This study had a sample size of 298 AD patients of varying severities; however, there was no indication toward the relative severity of patients in each group. It also does not disclose the number of locations that data was collated at which makes it difficult to compare different approaches to AD with this data due to an increased risk of bias. This is a repeated flaw in the RCT by Gomez-Gallego M et al., as the sample size was only 90 AD patients. In contrast, the presence of allocation bias was removed as the article directly informs the reader that the candidates selected came from 6 different nursing homes, hence reducing any unrelated anomaly-causing variables. Analysis of the results showed that active music intervention improved cognition, behaviour, and functional state in a higher extent than both receptive music intervention and usual care. This research is also more valid to the study as it is supported by a numerical indicator of the level of improvements in patients in each participant which increases the accuracy and precision of results [9].
The statistical significance of this data is clear when compared to Table 1 below. This quantitative data allows us to formulate a much more definitive, evidence-based conclusion on the effectiveness of musical therapy on treating Alzheimer’s symptoms and which specific type of musical therapy works most efficiently. Critically, despite the smaller sample size, the data seen in Figures 2-4 is superior to that of Lyu J et al., due to the absence of quantitative data in the latter study (Table 2) [10].
| Factors determining severity of Alzheimer's disease | Alzheimer's disease patients displaying improvement (%) | Alzheimer's disease patients displaying no change (%) |
|---|---|---|
| Cognitive deficits | 6.3 | 93.8 |
| Behavioural symptoms | 12.2 | 87.8 |
| Functional state | 17.1 | 82.9 |
Table 1: Indicating the percentage of Alzheimer’s disease patients with improved cognitive deficits, behavioural symptoms, and functional state (control group)
Figure 2) Effect of active music intervention on improved cognitive deficits in AD patients
Figure 3) Effect of active music intervention on improved behavioural symptoms in AD patients
Figure 4) Affect of active music intervention on improved functional state in AD patients
| Factors determining severity of Alzheimer's disease | Alzheimer's disease patients displaying improvement (%) | Alzheimer's disease patients displaying no change (%) |
|---|---|---|
| Cognitive deficits | 11.8 | 88.2 |
| Behavioural symptoms | 42.9 | 57.1 |
| Functional state | 14.3 | 85.7 |
Table 2: Indicating the percentage of alzheimer’s disease patients with improved cognitive deficits, behavioural symptoms, and functional state (receptive listening group)
Results and Discussion
An opposed option to using donepezil therapeutically for AD is the use of memantine. McShane R et al. concluded that the positive effects of memantine are dependent on the stage of AD in each patient. Results show that memantine has a small beneficial effect in people with moderate-to severe AD and in people with mild AD, memantine is probably no better than placebo [11]. This evidence was collated from 29 studies in 7885 people with AD in RCTs. This gives credibility to the author as the method of acquiring data is appropriate to ensure the outcome gives a fair reflection and helps minimise the risk of an outlier skewing the results. An issue with memantine compared to donepezil or music therapy is its specificity as the above study only found evidence of a positive reaction to the drug in patients with early-stage AD. Despite the author opting for the preferred method of assimilating a testing group, the evidence received for using memantine for treating mild AD is weak although this result seems to be a common trend. The comparison of these findings with another study shows unremarkable differences in results as it found memantine is effective in treating and preventing the behavioural symptoms of moderate to severe AD [12]. This trial was conducted with 1826 patients with moderate-to severe AD from 6 double-blind RCTs spanning 24-28 weeks which gives me complete assurance that the information recorded is high in integrity however, the author does not directly state that there are no known conflicts of interest with the study which does leave some uncertainty as to whether the article is as perfectly secure as it can be. Collectively, these documents do confirm a conclusive outcome of using memantine in patients with moderate-to-severe AD. Unfortunately, as it shows little to no benefit in mild AD patients, memantine is not the most viable option for preventing symptoms or reducing the rapid deterioration associated with worsening Alzheimer’s [13].
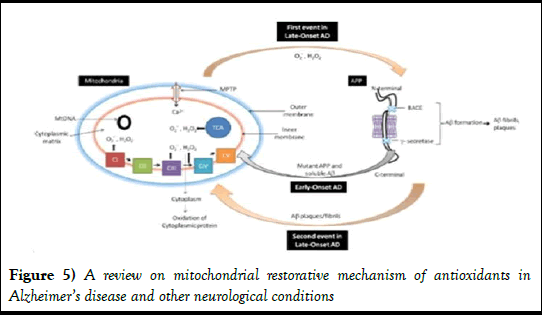
Alternative approaches to the treatment of Alzheimer’s also include the supplementation of coenzyme Q10. Coenzyme Q10 is a vitamin-like substance of vital importance for normal mitochondrial function and as an antioxidant. Schinder et al., states glutamate mitochondrial dysfunction is a primary event in glutamate neurotoxicity. The antioxidant effect of coenzyme Q10 prevents free radical formation in the mitochondria which can be seen in Figure 5 below. This is significant as free radicals accept electrons and cause oxidative stress, leading to mitochondrial dysfunction. As astrocytic mitochondria specifically become dysfunctional, glutamate concentrations in astrocytes increase.
Figure 5) A review on mitochondrial restorative mechanism of antioxidants in Alzheimer’s disease and other neurological conditions
This increased level of glutamate causes excitotoxicity across neurons initiates activation of the pro-apoptotic pathway leading directly to the symptoms associated with AD. This process is reduced due to coenzyme Q10’s antiapoptotic activity by inhibiting activation of the mitochondrial permeability [14]. The approach of using coenzyme Q10 supplements is safer than pharmaceutical methods as coenzyme Q10 is a naturally occurring substance and can be obtained from a balanced diet in most individuals through foods such as oily fish (salmon/tuna), organ meats (liver), and whole grains and thus meaning it does not cause side effects. Overall, the evidence associated with these findings may not be efficiently comparable as it is qualitative however; the known effects of natural Coenzyme Q10 mean the data is stronger as it is simply an enhancement of a natural process thus removing bias. This rationale of using mitochondrial targeting antio-xidative compounds to reduce the cognitive effects of Alzheimer’s is the same rationale used by other alternative methods e.g. Ginkgo biloba extract to improve memory problems. Another alternative treatment for AD is electro acupuncture. In acupuncture, fine needles are inserted at certain sites in the body for therapeutic or preventative purposes. Electro acupuncture follows the same principle however an electrical current is passed between needles [15]. The use of electro acupuncture for AD is to reduce glial/microglial cells activation and polarization into different phenotypes in neuro degeneration. In acute inflammation, the CNS undergoes rapid activation of glial cells in response to irritants such as toxic levels of proteins that contribute to neurodegenerative disease e.g. amyloid and tau. The normal activation of said glial cells mediates repair of damaged areas in the brain. The importance of preventing the over activation of glial cells is significant because over activation leads to neural tissue degeneration. A study into the use of electro acupuncture using 20 male Sprague-Dawley rats with AD concluded that electro acupuncture improves the recognition abilities and memory in AD rats. Results can be seen below (Tables 3 and 4) [16]. Thesignificance of this data is that there is a well-established correlation between the use of electro acupuncture and reduced neurological damage caused by overstimulation of glial cells in acute inflammatory response.
|
|
Activation of astrocytes and microglia |
Polarisation of microglia |
Glial inflammatory response |
|---|---|---|---|
|
Change when compared to control (+/-) |
Increase (+) |
Significant increase (+) |
Increase (+) |
Table 3: Assessment of the effects of electro acupuncture on the neurological processes in sprague-dawley rats with Alzheimer’s disease ad rats with no electro acupuncture
|
|
Activation of astrocytes and microglia |
Polarisation of microglia |
Glial inflammatory response |
|---|---|---|---|
|
Change when compared to control (+/-) |
Decrease (-) |
Decrease (-) |
Decrease (-) |
Table 4: Assessment of the effects of electro acupuncture on the neurological processes in sprague-dawley rats with Alzheimer’s disease ad rats with acupuncture
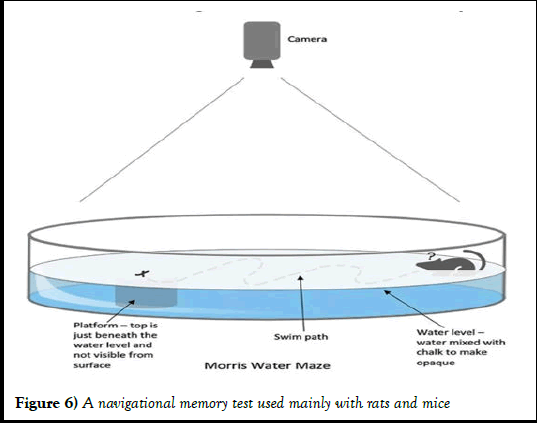
From a critique aspect, this data is invalid as the study is only in rats and may not have the same desired effect in humans and therefore makes it difficult to compare as an alternative treatment. Furthermore, the sample group contained 20 rats with only 5 under the influence of electro acupuncture [17,18]. These rats were also all male which, although does show a fair comparison between each subject in the study, does not show a representative result across both male and female rats which may result in anomaly. Finally, this data looks at the ability of each rat to complete the Morris Water Maze, seen in Figure 6. The rats navigate through an opaque water-bath to find a submerged platform as quickly as possible from memory. The quantitative results were not published for comparison between rats which makes it difficult to have confidence in the data as we cannot determine how significant the effects of the electro acupuncture is.
Figure 6) A navigational memory test used mainly with rats and mice
Conclusion
Upon analysis, I conclude that the most effective methods for treating Alzheimer’s are pharmaceutical. This is due to the strength of the data’s credibility obtained through the RCT method of data collection as well as larger sample sizes and more transparent results of the study. Although drugs can display side-effects and are not entirely suitable for all stages of AD patients (e.g. lack of efficacy of Memantine in mild AD patients), each study regarding pharmaceutical approaches showed stronger evidence of benefit in human use and overall acts on the pathophysiological processes in an attempt to reduce the effects of AD rather than acting on contributing factors. Alternative therapies had several limitations including a lack of numerical data, non-RCT trials and no human trial data which makes these studies a less reliable source of data when comparing treatment of AD.
References
- Alzheimer's Research UK. The word dementia is used to describe a group of symptoms including memory loss, confusion, and communication difficulties. 2019.
- Alzheimer's Society. Alzheimer’s society’s view on demography. Alzheimer’s Society. 2019.
- Arvanitakis Z, Shah RC, Bennett DA. Diagnosis and management of dementia. JAMA. 2019;322(16):1589-99.
[Crossref] [Google Scholar] [PubMed]
- Birks J, Craig D. Galantamine for vascular cognitive impairment. Cochrane Database Syst Rev. 2006(1).
[Crossref] [Google Scholar] [PubMed]
- Birks JS, Harvey RJ. Donepezil for dementia due to Alzheimer's disease. Cochrane Database of systematic reviews. 2018(6).
[Crossref] [Google Scholar] [PubMed]
- Gauthier S, Loft H, Cummings J. Improvement in behavioural symptoms in patients with moderate to severe Alzheimer's disease by memantine: A pooled data analysis. Int J Geriatr Psychiatry. 2008;23(5):537-45.
[Crossref] [Google Scholar] [PubMed]
- Gomez-Gallego M, Gomez-Gallego JC, Gallego-Mellado M, et al. Comparative efficacy of active group music intervention versus group music listening in Alzheimer’s disease. Int J Environ Res Public Health. 2021;18(15):8067.
[Crossref] [Google Scholar] [PubMed]
- Goubert E, Mircheva Y, Lasorsa FM, et al. Inhibition of the mitochondrial glutamate carrier SLC25A22 in astrocytes leads to intracellular glutamate accumulation. Front Cell Neurosci. 2017;11:149.
[Crossref] [Google Scholar] [PubMed]
- Kumar A, Singh A. A review on mitochondrial restorative mechanism of antioxidants in Alzheimer’s disease and other neurological conditions. Front Pharmacol. 2015;6:206.
[Crossref] [Google Scholar] [PubMed]
- Luengo-Fernandez R, Leal J, Gray A. UK research spend in 2008 and 2012: comparing stroke, cancer, coronary heart disease and dementia. BMJ open. 2015;5(4):e006648.
[Crossref] [Google Scholar] [PubMed]
- Lyu J, Zhang J, Mu H, et al. The effects of music therapy on cognition, psychiatric symptoms, and activities of daily living in patients with Alzheimer’s disease. J Alzheimers Dis. 2018;64(4):1347-58.
[Crossref] [Google Scholar] [PubMed]
- Mantle D, Heaton RA, Hargreaves IP. Coenzyme Q10, ageing and the nervous system: an overview. Antioxidants. 2021;11(1):2.
[Crossref] [Google Scholar] [PubMed]
- Matthews RT, Yang L, Browne S, Baik M, Beal MF. Coenzyme Q10 administration increases brain mitochondrial concentrations and exerts neuroprotective effects. Proc Natl Acad Sci U S A. 1998;95(15):8892-97.
[Crossref] [Google Scholar] [PubMed]
- McShane R, Westby MJ, Roberts E, et al. Memantine for dementia. Cochrane Database Syst Rev. 2019;3(3):CD003154.
[Crossref] [Google Scholar] [PubMed]
- Revett TJ, Baker GB, Jhamandas J, et al. Glutamate system, amyloid β peptides and tau protein: Functional interrelationships and relevance to Alzheimer disease pathology. J Psychiatry Neurosci. 2013;38(1):6-23.
[Crossref] [Google Scholar] [PubMed]
- Saini R. Coenzyme Q10: The essential nutrient. J Pharm Bioallied Sci. 2011;3(3):466-7.
[Crossref] [Google Scholar] [PubMed]
- Sochocka M, Diniz BS, Leszek J. Inflammatory response in the CNS: friend or foe?. Mol Neurobiol. 2017;54:8071-89.
[Crossref] [Google Scholar] [PubMed]
- Wang R, Reddy PH. Role of glutamate and NMDA receptors in Alzheimer’s disease. J Alzheimers Dis. 2017;57(4):1041-48.
[Crossref] [Google Scholar] [PubMed]