Bilioptysis with hepatobiliobron chial fistula: A rare hepatic hydatidosis complication
2 Department of Gastrointestinal Surgery, Virgen of the Macarena, Seville, Spain
Received: 30-Oct-2018 Accepted Date: Nov 01, 2018; Published: 05-Nov-2018
Citation: Luque JB, Redondo AR, Sanchez-Matamoros I, et al. Bilioptysis with hepatobiliobronchial fistula: A rare hepatic hydatidosis complication. Surg Case Rep. 2018;2(2):35-36.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
We present a case of a patient with hepatic hydatidosis who, after an episode of cholangitis, presented bilioptysis. A biliobronchial fistula and portal thrombosis were diagnosed, requiring surgical fistula resection and bile duct prostheses placement as well as a vena cava filter. After the procedure, the patient has not relapsed and continues with a vena cava filter due to his portal thrombosis.
Keywords
Biobronchial fistula; Hepatic hydatidosis; Bilioptysis; Right hepatectomy
Introduction
The Biliobronchial Fistula (BBF) is a rare communication between the biliary tract and the bronchial tree [1]. The most frequent acquired causes are the rupture of hydatid cysts, hepatic abscesses, trauma or iatrogenesis, being the congenital ones extremely rares [2]. The prevalence estimated in a series of cases is 3.5% [3]. The most frequent symptomatology is bilioptysis, being or not accompanied by cough, fever, jaundice, abdominal and thoracic pain, nausea and vomiting [4,5]. Early diagnosis is important for further treatment due to difficult management. Magnetic resonance cholangiography and CT scan are useful in this pathology [6] although the demonstration of bilirubin in sputum is a cost-effective measure as the first choice [1]. There are different treatments for biliobronchial fistula, being invasive procedures the last option in this type of patient [6].
Case Presentation
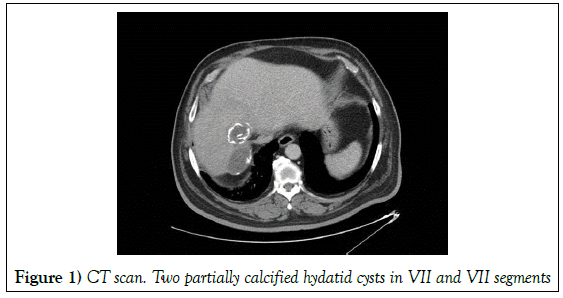
A 68-year-old man with history of type II Diabetes Mellitus, moderate renal insufficiency, Hypertension and previous cholecystectomy, was admitted into Emergency department due to episode of cholangitis caused by streptococcus anginosus. During admission in the Digestive Unit, complementary tests were performed, observing two 4.5 cm and 5.5 mm hydatid cysts in VIII and VII liver segments respectively, with aerobilia and portal thrombosis (Figure 1).
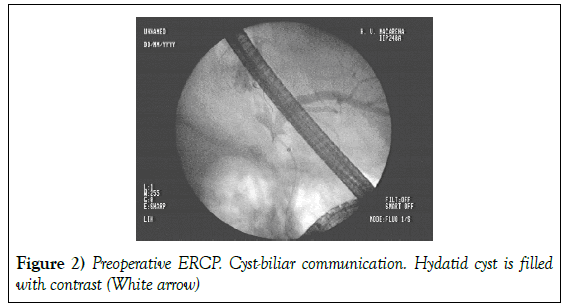
An Endoscopic Cholangiopancreatography (ERCP) was performed and a communication with the biliary tract is visualized, proceeding to perform sphincterotomy and biliary lavage with good results (Figure 2). The cholangitis was solved, and the patient was discharge after two weeks. The following year the patient was admitted again due to vomiting and fever with initial diagnosis of basal pneumonia due to right pulmonary mass, ruling out malignancy.
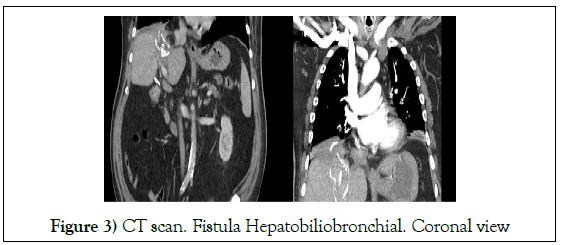
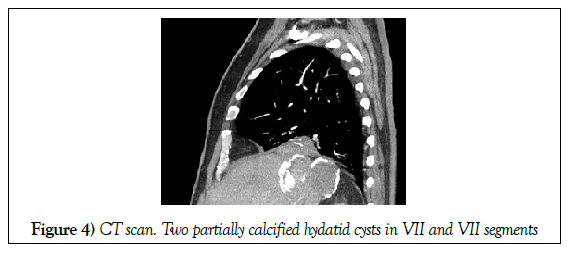
In the CT scan performed during admission, pulmonary thromboembolism (PTE) was observed with a large thrombus in the right pulmonary artery. After anticoagulation, the PTE was solved but he kept presenting vomiting. A bilioptysis was suspected and a sputum biochemistry was performed, finding a bilirubin of 2 mg / dl. The diagnosis of Biliobronchial fistula was confirmed (Figures 3 and 4).
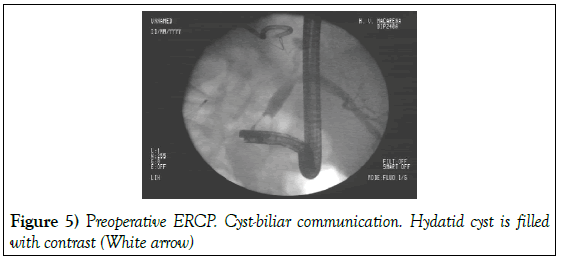
A scheduled surgery is proposed. The patient undergone to right hepatectomy with diaphragmatic 90 gap closure and percutaneous drain placement as well as an inferior vena cava filter. During postoperatory course, a persistent bile leak is shown through the drain, and ERCP was performed, identifying the leakage coming from the liver resection margin (Figure 5).
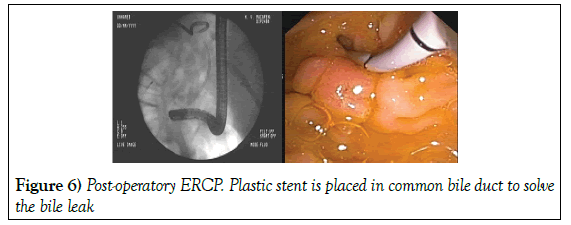
The bile leak is solved with a plastic stent placement that was removed at 6 months (Figure 6).
After the prosthesis removal, the patient presents episodes of deep venous thrombosis in both legs, so he continues with an inferior vena cava filter. Currently the patient remains with good general condition and favorable evolution after two years follow-up. The histopathology was discussed with multidisciplinary team including the pediatric oncology team. Ultrasound (USG) abdomen ruled out other associated intra-abdominal pathology. In view of complete surgical resection and type 1 of pleuro pulmonary blastoma child was advised regular follow up without any adjuvant chemo or radiotherapy. At the end of one year follow up, the child is doing well with no evidence of local recurrence.
Discussion
Biliobronchial fistula is an infrequent pathology that arises as a complication, in our case, of a hydatid cyst that has been asymptomatic for years but is complicated by an episode of cholangitis. The early diagnosis of this pathology is a fundamental pillar. The clinical diagnosis has vital importance, being the bilioptysis the pathognomonic symptom of this pathology as in the case of our patient. Sputum analysis helps to confirm the diagnosis to proceed to more effective targeted treatment. Among the most frequent diagnostic imaging are CT scan and ERCP, both performed in our patient. The ERCP has high relevance in this patient due to the therapeutic attitude with the previous cholangitis and post-operatory bile leak. There isn´t a gold standard in BBF treatment due to the few studies carried out and low evidence that is currently available. The treatment should be tailored according to each patient. Among the non-surgical therapeutic options are the placement of metallic or plastic biliary stent and fistulous tract embolization. However, there is low experience with these methods and some experts recommend only the placement of endoprostheses as exclusive treatment in patients with low life expectancy.
Conclusion
Surgical invasive treatment should always be the last option but must be taken into consideration whenever necessary. In our case, right hepatectomy with diaphragmatic gap closure were performed to solve the thoracic transit. Therapeutic ERCP with biliary stent placement is useful in post-operatory bile leak after hepatectomy.
REFERENCES
- Nassar Y, Hida S, Richter S. A biliobronchial fistula in a patient with hepatocellcular carcinoma treated with chemoembolization diagnosed by hepatobiliary iminodiacetic acid scan and managed by endoscopic retrograde cholangiopancreatography. Gastroenterology Res. 2017;10(6):383-385.
- Chautems R, Buhler LH, Gold B, et al. Surgical management and long-term outcome of complicated liver hydatid cyst caused by Echinococcus granulosus. Surgery 2005;137: 326-28.
- Uchikov AP, Safev GP, Stefanov CS, et al. Surgical treatment of bronchobiliary fistulas due to complicated echinococcosis of the liver: case report and literature review. Folia Med (Plovdiv) 2005;45(4):22-24.
- Sahin E, Enon S, Cangir AK, et al. Single-stage transthoracic approach for right lung and liver hydatid disease. J Thorac Cardiovasc Surg 2003;126(3):769-773.
- Losada H, Vial M, Manterola C, et al. Bronchobiliary fistula secondary to a hepatic hydatid cyst in transit to the thorax. Report of one case. Rev. Chilena de CirugÃÂa. 2006:58(3)224-227.
- Liao GQ, Wang H, Zhu GY, et al. Management of acquired bronchobiliary fistula: A systematic literature review of 68 cases published in 30 years. World J Gastroenterol. 2011;17(33):3842-3849.