Hemobilia from rupture of pseudoaneurysm on right hepatic artery after cholecystectomy - a case report
2 Damascus University Faculty of Medicine, Damascus, Syrian Arab Republic, Email: fadirayya@yahoo.com
Received: 31-May-2018 Accepted Date: Jun 12, 2018; Published: 18-Jun-2018
Citation: Rayya F, Ghanem M, Ahmad A, et. al.. Hemobilia from rupture of pseudoaneurysm on right hepatic artery after cholecystectomy - a case report. General Surgery: Open Access. 2018;1(1):19-21.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Background: Iatrogenic etiologies are currently the leading causes of hemobilia, which is a life-threatening case.
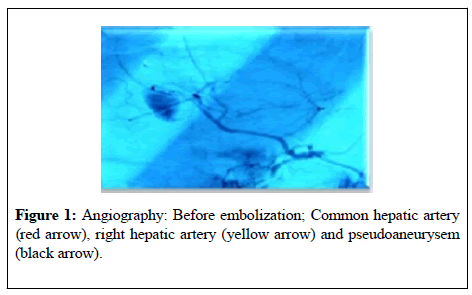
Case presentation: We present a case of hemobilia after laparoscopic cholecystectomy in which an injury to the biliary system happened, and then the patient had the clinical descriptive triad of hemobilia "Quinke triad" which includes pain, gastrointestinal bleeding and jaundice. Gastrointestinal endoscopy led us to think of hemobilia; using angiography we discovered a pseudoaneurysm on the right hepatic artery. Our expert emobolized the aneurysm using the interventional radiology, the patient was fully recovered.
Results: Regardless of the date of surgery, thinking of hemobilia as a complication after a cholecystectomy in the complains of any patient of gastrointestinal bleeding is considered. It is essential to have an upper gastrointestinal endoscopy. Initial management includes an appropriate resuscitation with IV fluids. Angiographic CT might be useful to locate the source of the bleeding for early and appropriate targeted therapy.
Keywords
Hemobilia; pseudoaneurysm of right hepatic artery; cholecystectomy; embolization; interventional radiology
Introduction
Hemobilia is a case in which the bleeding results from a connection between the vascular and biliary systems. Historically it was associated with external trauma both penetrating and blunt. With the rise of medical interventional techniques on biliary systems, iatrogenic hemobilia comprises over 70% of all cases. Although it is more common in PTBD, PTC and liver biopsies, we present a case of pseudoaneurysm of the right hepatic artery leading to hemobilia after rupturing into the biliary tract.
Case Report
A 34 years old male patient presented to our clinic at Al-Assad university hospital complaining of abdominal pain after a blood splash flew out from his T-tube which was put after a cholecystectomy that turned into open surgery because of an injury to the biliary tract 2 months ago.
The patient mentioned that he had a colic abdominal pain, jaundice and a story of melena and hematemesis.
By reviewing the medical history we noticed that the patient had had an ERCP because of common bile duct stones then he went a laparoscopic cholecystectomy that turned into an open surgery because of an injury to the biliary tract. The injury was treated with initial suture, then a drain was put near the injury site without having a T-tube put into the biliary tract (it was not available at hospital that time). The drain continued to produce large amounts of bile daily. One week after surgery the patient developed jaundice. Abdominal ultrasound showed large amounts of thick liquid in pelvic cavity. The patient underwent another surgery in which the liquids were suctioned and a T-tube was placed into the common bile duct (CBD).
The patient mentions that the T-tube produced a splash of fresh blood twice (the first happened after a cholangiography through the T-tube, and the second occurred after a T-tube closure test).
He had an upper gastrointestinal endoscopy (gastrointestinal haemorrhage), it revealed a blood clot in gastric funds with fresh blood clot in the second part of the duodenum, hemobilia was suspected.
When the patient arrived to our hospital he was jaundiced, his pulse was 120 hpm, and his blood pressure was 90/60 mmHg with no change in mental status, abdominal examination was normal.
Laboratory
Hb:9.8, HCT:29, TB:7.6, DB:5.1, ALP:101, ALT:56, AST:62
The initial management was to transfer two units of blood and two of fresh frozen plasma (FFP). An abdominal ultrasound was done; it demonstrated the presence of saccular formation in gallbladder bed in which blood flow was noticed.
Then an angiographic Multi Slice CT (MSCT) was done, it revealed the presence of mixed density gathering in the lesser momentum below the diaphragm compressing stomach and left hepatic lobe measures 10 x 2 cm which represents hematoma. Also, a dilated area at the end of the hepatic artery was noticed that represents an aneurysm measures 2.8 cm in the helium of liver.
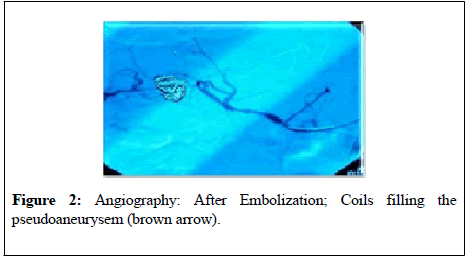
Patient consent was ensured to have an aneurysm embolization. Our interventional radiologist embolized the aneurysm using 2 coils of 4 x 12 and one coil of 3 x 8 (MedTronic-USA) after the catheterization of the right hepatic artery using the Seldingers technique.
The patient was discharged 3 days after embolization in a good status, and he is being routinely followed up with no complications.
Discussion
Hemobilia is defined as haemorrhage into the biliary tract from an abnormal connection between the splanchnic circulation and bile ducts.
Francis Glisson was the first to describe hemobilia in 1654 in a young male patient who was stabbed in the right hypochondrium which led to severe hematemesis that seemed to originate from a deep laceration of the liver at post-mortem examination [1,2]. Historically Heinrich Quincke described the triad of symptoms associated with hemobilia in 1871 including pain, gastrointestinal bleeding and jaundice. However, less than 40% of the cases present with the complete triad [2,3] and in our case our patient has suffered this triad.
The term hemobilia was first used to describe haemorrhage into the biliary tract after blunt trauma in 1984 by Philb Sandblom [1,3].
Hemobilia was more common in traumatic patients accounting for 30% of all cases followed by chololithiasis 15% inflammation 13% vascular etiologies 10.7% and then oncogenic 6.2% [4].
Iatrogenic hemobilia is currently more frequent and comprises over 70% of all cases. According to many studies the risk of developing hemobilia occurs in 2% of the cases after PTBD, in less than 1% after PTC [5], and rarely happens after liver biopsy [6].
Pseudoaneurysm of hepatic artery may arise as a complication of laparoscopic cholecystectomy because of clip encroachments, mechanical or thermal injury during the procedure [7].
The right hepatic artery is the most common site among all hepatic artery pseudoaneurysm accounting for almost 80% of the cases [8]. One rare case report described a pseudoaneurysm formation on cystic artery with the presence of anatomic variation (right hepatic artery originates from SMA) which made it easier to have the aneurysm embolized.
The presence of bile is known to damage blood vessels, so simultaneous injury to biliary structures can delay healing of an injured artery and predispose the formation of pseudoaneurysms [9,10]. We have seen in the case of our patient that bile leakage continued to flow from the tubular drainage (after his first operation) for a whole week in large amounts which contributed to pseudoaneurysm formation. It is clear that good drainage to biliary tract, by putting a T-tube, after any injury is so important taking into consideration that stopping haemorrhage is the first purpose.
Hemobilia could cause biliary obstruction. Endoscopy is administered to relief the pressure in bile ducts [11].
Gastrointestinal endoscopy could confirm the diagnosis of hemobilia in 10% of cases [12], and it is considered mandatory in the evaluation of patient presenting with symptoms of gastrointestinal haemorrhage, it can rule out other causes of haemorrhage [13,14]. In fact it was the main diagnostic tool used in the case of our patient to suggest hemobilia.
Abdominal sonography (Echo) and echo Doppler are useful diagnostic investigations for initial evaluation of hemobilia. Sonographic features may include dilation of the common bile duct which was reported to be present in 28% of cases [15].
Today CT is increasingly being used to evaluate hemobilia which is considered to be useful to identify the predisposing factors such as tumors, inflammation and pseudoaneurysms [16].
Selective right hepatic angiography remains vital in the diagnosis of upper GI bleeding haemorrhage and it is useful to direct the following therapeutic procedure [17].
Embolization offers the advantage of minimally invasive treatment in the hemodynamically unstable patients and it is an effective treatment for this potentially life-threatening complication [18]. Success rates using TAE is 80-100% [19] (Figure 1).
By reviewing literature many cases of hemobilia were reported some of which were treated by embolization while others underwent surgery. One case of hemobilia happened two years after open cholecystectomy, significantly GI endoscopy was negative but two micro aneurysms were noticed through angiography, they were embolized with coils. The patient was fully recovered [20] (Figure 2).
Coils embolization was reported to be used in a rare case of hemobilia caused by a pseudoaneurysm on the cystic artery. It was done successfully, the patient then went through a cholecystectomy [21].
A similar case report of hemobilia was published in the department of abdominal surgery in Vladimir city Clinical hospital of Emergency medicine, Russia, Trans arterial embolization of the right hepatic artery using polyvinyl alcohol particles was performed. Recurrent hemobilia was diagnosed 6 days after TAE; the patient underwent urgent laparotomy and ligation of right hepatic artery [22].
The major disadvantages of polyvinyl alcohol particles are their tendency to aggregate, occluding vessels more proximally than might be expected based on stated size and the possible recanalization of the embolus [23,24]. In the case of our patient we used coils and no complications occurred as a result.
TAE is the gold standard to manage hemobilia caused by pseudoaneurysm. In case of failing or absence of embolization, the next step is surgery which permits direct exploration and possible hepatic resection or packing, aneurysm excision, cholecystectomy and relief of bile obstruction. In some other cases surgical intervention was used after failure of embolization [20].
Conclusion
Vascular complications after laparoscopic cholecystectomy should be observed carefully especially when GI haemorrhage develops. Pseudo aneurysms formation might be the cause.
Initial management includes resuscitation with IV fluids. GI endoscopy then should be performed to rule out other causes of bleeding. Angiography is a good diagnostic and therapeutic tool. TAE is the golden standard to manage pseudoaneurysm, and in case of failure or absence of TAE, surgery is the next step.
REFERENCES
- Green MH, Duell RM, Johnson CD, et al. Br J Surg 2001;88(6):773-86.
- Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery 1948;24(3):571-86.
- Glisson F. Anatomia Hepatis. Cui Preamittuntur Quaedam Ad Rem Anatomican Universe Spectantia, Amsterdam. 1597-1677.
- Sandblom P. Hemobilia (biliary tract hemorrhage): history, pathology, diagnosis, treatment. 1972.
- Fidelman N, Bloom AI, Kerlan RK, et al. Hepatic Arterial Injuries after Percutaneous Biliary Interventions in the Era of Laparoscopic Surgery and Liver Transplantation: Experience with 930 Patients. Radiology 2008;247(3):880-6.
- Piccinino F, Sagnelli E, Pasquale G, et al. Complications following percutaneous liver biopsy. A multicentre retrospective study on 68,276 biopsies. J Hepatol 1986;2(2):165-73.
- Curet P, Baumer R, Roche A, et al. Hepatic hemobilia of traumatic or iatrogenic origin: recent advances in diagnosis and therapy, review of the literature from 1976 to 1981. World J Surg 1984;8(1):2-8.
- Tessier DJ, Fowl RJ, Stone WM, et al. Iatrogenic Hepatic Artery Pseudoaneurysms: An Uncommon Complication after Hepatic, Biliary, and Pancreatic Procedures. Ann Vasc Surg 2003;17(6):663-9.
- Vachhani PG, Copelan A, Remer EM, et al. Iatrogenic hepatopancreaticobiliary injuries: a review. Semin Intervent Radiol 2015;32(2):182-94.
- Madanur MA, Battula N, Sethi H, et al. Pseudoaneurysm following laparoscopic cholecystectomy. Hepatobiliary Pancreat Dis Int 2007;6(3):294-8.
- Kim KH, Kim TN. Etiology, clinical features, and endoscopic management of hemobilia: a retrospective analysis of 37 cases. Korean J Gastroenterol 2012;59(4):296-302.
- Senadhi V, Arora D, Arora M, et al. Hemobilia caused by a ruptured hepatic cyst: a case report. J Med Case Rep 2011;5(1):26.
- Yoshida J, Donahue PE, Nyhus LM. Hemobilia: review of recent experience with a worldwide problem. Am J Gastroenterol 1987;82(5):448-53.
- Murugesan SD, Sathyanesan J, Lakshmanan A, et al. Massive hemobilia: a diagnostic and therapeutic challenge. World J Surg 2014;38(7):1755-62.
- Laing FC, Frates MC, Feldstein VA, et al. Hemobilia: sonographic appearances in the gallbladder and biliary tree with emphasis on intracholecystic blood. J Ultrasound Med 1997;16(8):537-43.
- Feng W, Yue D, ZaiMing L, et al. Iatrogenic hemobilia: imaging features and management with transcatheter arterial embolization in 30 patients. Diagn Interv Radiol 2016;22(4):371-7.
- Horton KM, Smith C, Fishman EK. MDCT and 3D CT Angiography of Splanchnic Artery Aneurysms. Am J Roentgenol 2007;189(3):641-7.
- Nicholson T, Travis S, Ettles D, et al. Hepatic artery angiography and embolization for hemobilia following laparoscopic cholecystectomy. Cardiovasc Intervent Radiol 1999;22(1):20-4.
- Sibulesky L, Ridlen M, Pricolo VE. Hemobilia due to cystic artery pseudoaneurysm. Am J Surg. 2006;191(6):797-8.
- Liu Z, Yang S, Xi P. An Unusual Life-Threatening Hemobilia Caused by Hepatic Pseudoaneurysm Following Choledochostomy: A Case Report. Case Reports Clin Med 2016;05(02):37-42.
- Trombatore C, Scilletta R, Bellavia N, et al. Acute hemobilia from a pseudoaneurysm of the cystic artery arising from the left hepatic artery: Case report and literature review. Int J Surg Case Rep 2017;37:60-4.
- Gachabayov M, Kubachev K, Mityushin S, et al. Recurrent Hemobilia Due to Right Hepatic Artery Pseudoaneurysm. Clin Med Res 2017;15(3-4):96-9.
- Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol 2008;25(3):204-15.
- Lubarsky M, Ray CE, Funaki B. Embolization agents-which one should be used when? Part 1: large-vessel embolization. Semin Intervent Radiol 2009;26(4): 352-7.