Small concept dealing with diabetic retinopathy
Received: 07-Jan-2022, Manuscript No. puljpl-22-3474; Editor assigned: 09-Jan-2022, Pre QC No. puljpl-22-3474(PQ); Accepted Date: Feb 07, 2022; Reviewed: 23-Jan-2022 QC No. puljpl-22-3474(Q); Revised: 28-Jan-2022, Manuscript No. puljpl-22-3474(R); Published: 07-Feb-2022
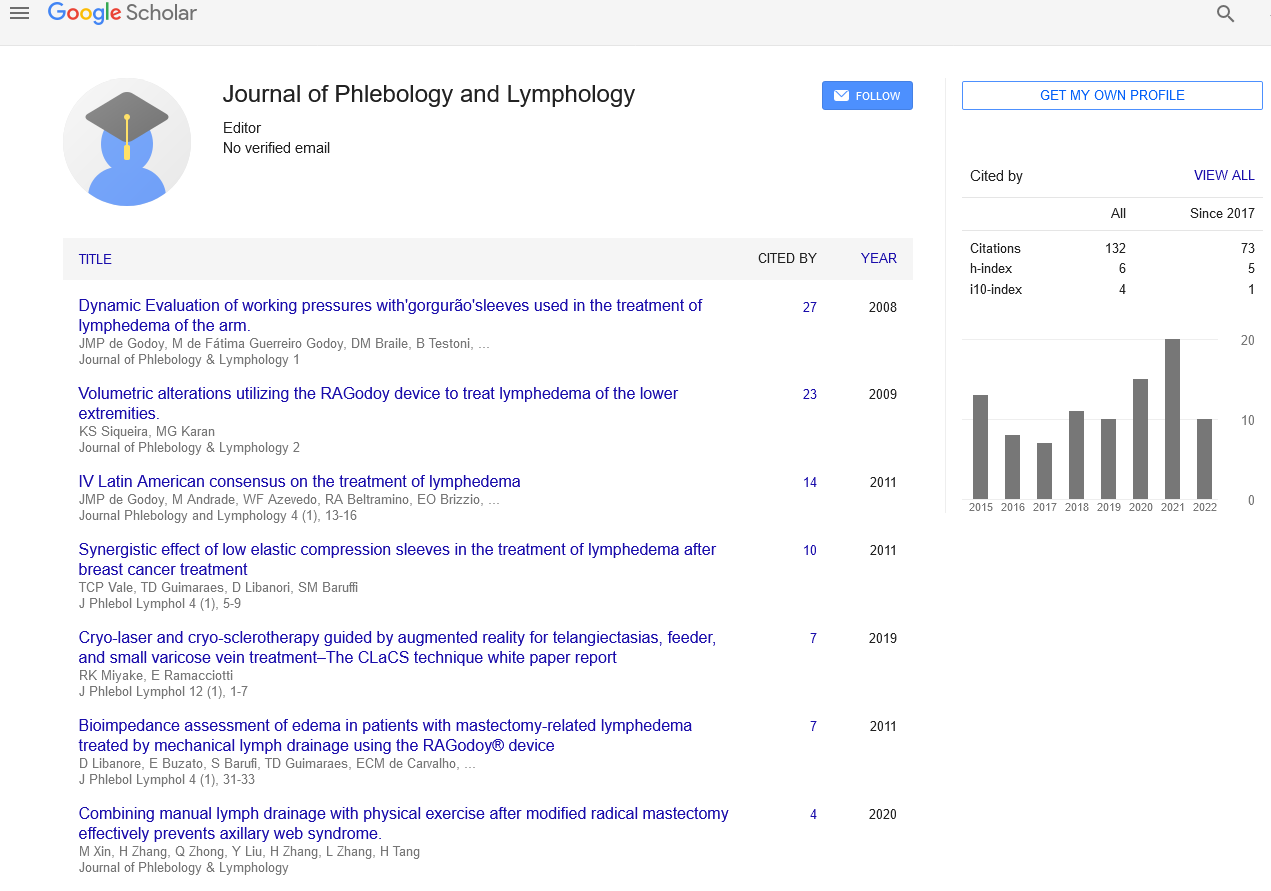
Citation: Shing L. Small concept dealing with diabetic retinopathy. J Phlebol Lymphology 2022;15(1):1-2
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Diabetic retinopathy, also known as diabetic eye disease (DED), is a medical condition in which damage occurs to the retina due to diabetes mellitus. It is a leading cause of blindness in developed countries. Diabetic retinopathy affects up to eighty percentages of those who have had diabetes for twenty years or more. At least ninety percentage of new cases could be reduced with proper treatment and monitoring of the eyes The longer a person has diabetes, the higher his or her chances of developing diabetic retinopathy Each year in the United States, diabetic retinopathy accounts for twelve percentages of all new cases of blindness. It is also the leading cause of blindness in people aged twenty to sixty-four year
Key Words
Vitreous haemorrhage; Neovascularisation; Proliferative diabetic Retinopathy; Angiopoietins
Introduction
Diabetic retinopathy often has no early warning signs. Even macular enema, which can cause rapid central vision loss, may not have any warning signs for some time. In general, however, a person with macular enema is likely to have blurred vision, making it hard to do things like read or drive. In some cases, the vision will get better or worse during the day
The first stage, called Non-Proliferative Diabetic Retinopathy (NPDR), has no symptoms. Patients may not notice the signs and have 0/0 vision. The only way to detect NPDR is by fundus examination by direct or indirect ophthalmoscope by a trained ophthalmologist, fundus photography can be used for objective documentation of the fundus findings, in which micro aneurysms (microscopic blood-filled bulges in the artery walls) can be seen. If there is reduced vision, fluorescein angiography can show narrowing or blocked retinal blood vessels clearly (lack of blood flow or retinal ischemia).
Method
Macular enema, in which blood vessels leak their contents into the macular region, can occur at any stage of NPDR. Its symptoms are blurred vision and darkened or distorted images that are not the same in both eyes. Ten present of diabetic patients will have vision loss related to macular enema. Optical Coherence Tomography can show areas of retinal thickening due to fluid accumulation from macular enema
In the second stage, abnormal new blood vessels (neovascularisation) form at the back of the eye as part of Proliferative Diabetic Retinopathy (PDR); these can burst and bleed (vitreous haemorrhage) and blur the vision, because these new blood vessels are fragile. The first time this bleeding occurs, it may not be very severe. In most cases, it will leave just a few specks of blood, or spots floating in a person’s visual field which may last for months
These spots are often followed within a few days or weeks by a much greater leakage of blood, which blurs the vision. In extreme cases, a person may only be able to tell light from dark in that eye. It may take the blood anywhere from a few days to months or even years to clear from the inside of the eye, and in some cases the blood will not clear. These types of large haemorrhages tend to happen more than once
On funduscopic exam, a doctor will see cotton wool spots, flame haemorrhages, and dot-blot haemorrhage.
All people with diabetes are at risk those with Type I diabetes and those with Type II diabetes. The longer a person has had diabetes, the higher their risk of developing some ocular problem. Between 0 and present of Americans diagnosed with diabetes have some stage of diabetic retinopathy? After years of diabetes, nearly all patients with Type I diabetes and of patients with Type II diabetes have some degree of retinopathy; however, these statistics were published in using data from four years earlier, limiting the usefulness of the research. The subjects would have been diagnosed with diabetes in the late 0s, before modern fast-acting insulin and home glucose testing
Prior studies had also assumed a clear glycaemic threshold between people at high and low risk of diabetic retinopathy.
Published rates vary between trials, the proposed explanation being differences in study methods and reporting of prevalence rather than incidence values.
During pregnancy, diabetic retinopathy may also be a problem for women with diabetes. NIH recommends that all pregnant women with diabetes have comprehensive eye examination.
People with Down syndrome, who have extra chromosome material, almost never acquire diabetic retinopathy. This protection appears to be due to the elevated levels of end statin an anti-antigenic protein, derived from collagen eighteen. The collagen eighteen genes are located on chromosome.
Genetics also play a role in diabetic retinopathy. Genetic predisposition to diabetic retinopathy in type diabetes consists of many genetic variants across the genome that are collectively associated with diabetic retinopathy (polygenic risk) and overlaps with genetic risk for glucose, low-density lipoprotein cholesterol, and systolic blood pressure.
Diabetic Retinopathy (DR) is the most common complication of Diabetes Mellitus (DM). It has long been recognized as a micro vascular disease. The diagnosis of DR relies on the detection of micro vascular lesions. The treatment of DR remains challenging. The advent of anti-Vascular Endothelial Growth Factor (VEGF) therapy demonstrated remarkable clinical benefits in DR patients; however, the majority of patients failed to achieve clinically-significant visual improvement. Therefore, there is an urgent need for the development of new treatments. Laboratory and clinical evidence showed that in addition to micro vascular changes, inflammation and retinal neurodegeneration may contribute to diabetic retinal damage in the early stages of DR. Further investigation of the underlying molecular mechanisms may provide targets for the development of new early interventions. Here, we present a review of the current understanding and new insights into pathophysiology in DR, as well as clinical treatments for DR patients. Recent laboratory findings and related clinical trials are also reviewed.
DR has long been recognized as a micro vascular disease. Hyperglycaemia is considered to play an important role in the pathogenesis of retinal micro vascular damage. Multiple metabolic pathways have been implicated in hyperglycaemia-induced vascular damage including the polyol pathway, Advanced Gyration End Products (AGEs) accumulation, the Protein Kinase C (PKC) pathway and the hexamine pathway
Conclusion
The earliest responses of the retinal blood vessels to hyperglycaemia are dilatation of blood vessels and blood flow changes. These changes are considered to be a metabolic auto regulation to increase retinal metabolism in diabetic subjects. Parricide loss is another hallmark of the early events of DR. Evidence of apoptosis of prices triggered by high glucose has been shown in both in vitro and in vivo studies, since prices are responsible for providing structural support for capillaries, loss of them leads to localized out pouching of capillary walls. This process is associated with micro aneurysm formation, which is the earliest clinical sign of DR. In addition to parricide loss, apoptosis of endothelial cells and thickening of the basement membrane are also detected during the pathogenesis of DR, which collectively contribute to the impairment of the BRB. Furthermore, pronounced loss of prices and endothelial cells results in capillary occlusion and ischemia. Retinal ischemia/ hypoxia leads to up regulation of VEGF through activation of Hypoxia Inducible Factor (HIF-). Other evidence suggested that Phospholipase A’s (PLA) elevation under the diabetic condition also triggers up regulation of VEGF 0. VEGF, a key factor involved in the progression of PDR and DME, is believed to increase vascular permeability by inducing phosphorylation of tight junction proteins such as occluding and Zonally Occludes- (ZO-). Moreover, as an antigenic factor, VEGF promotes proliferation of endothelial cells through activation of Mitogen-Activated Protein (MAP). Enhanced expression of VEGF has been detected in the retina of diabetic mouse, as well as the vitreous of patients with DME and PDR.
Other antigenic factors such as Angiopoietins (Ana, Nag-) are also involved in the regulation of vascular permeability by interacting with endothelial receptor tyrosine kinase Tie. Nag-, antagonist of Tie, has been shown to promote vascular leakage in the diabetic rat retina. It is speculated that antigenic factors besides VEGF might be involved in the alteration of microvasculature during DR; thus, they may provide novel therapeutic targets.