The inflammation hypothesis and mental illness
Received: 22-May-2019 Accepted Date: Jun 04, 2019; Published: 11-Jun-2019
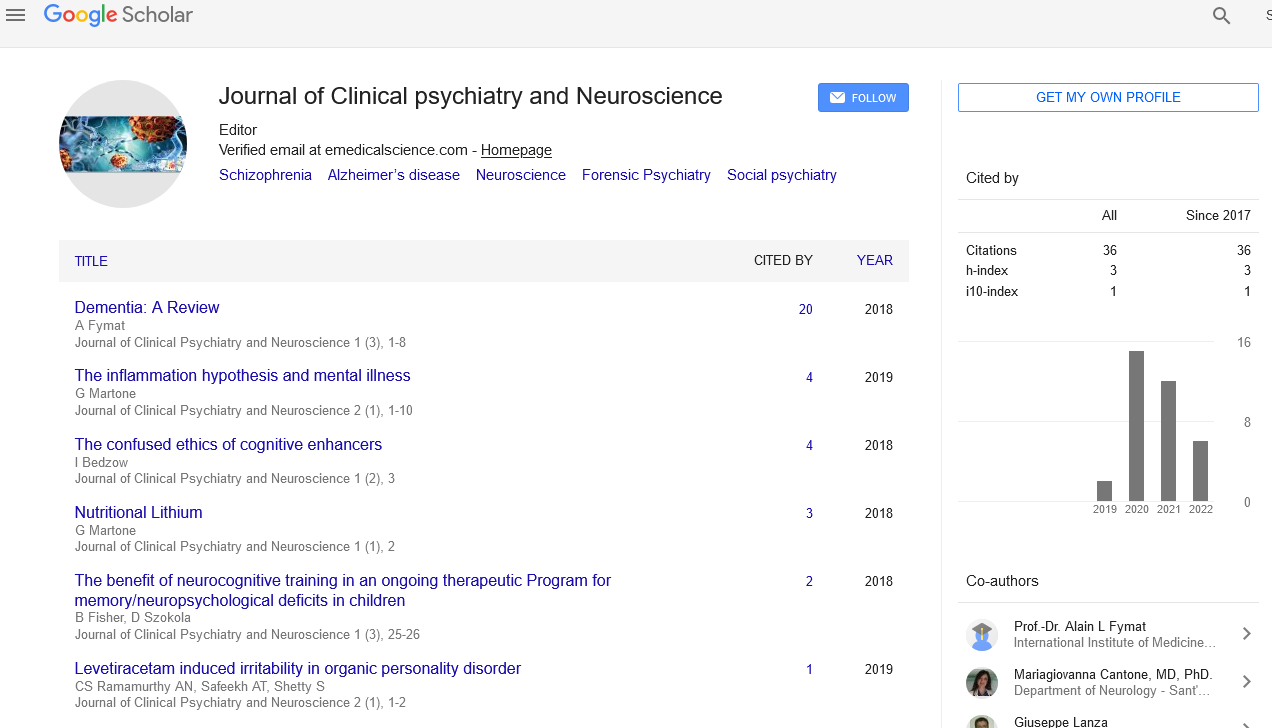
Citation: Martone G. The inflammation hypothesis and mental illness. J Clin Psychiatr Neurosci 2019;2(1):3-12.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Contemporary neuroscience and psychiatry are currently experiencing a rapid evolution. The foundations of these relatively new sciences are still largely theoretical and speculative. There are many competing hypotheses regarding the etiology and pathogenesis of mental illness. Unlike most somatic pathology, there is not a single laboratory test or objective disease marker for any psychiatric disorders. One of the dominant etiological paradigms in psychiatry involves the functional levels of neurotransmitters. Even this assumption is mootable, untestable, and widely disputed.
Several psychiatric disorders - Depression, Schizophrenia, Bipolar Disorder, Alzheimer’s disease, Traumatic Brian Injury, Autism, Parkinson’s disease, and Post-Traumatic Stress Disorder are associated with a dysregulation of immune responses and measurably increased inflammatory markers.
There is an empirical correlation of an over-activated immune system with the development of psychiatric symptomatology. By experimentally inducing systemic inflammation, cognition and behavior are adversely affected. By experimentally suppressing inflammation, sensorium and mood can be dramatically improved.
Anti-inflammatory agents such as NSAIDS (COX-2 inhibitors), low-dose Aspirin (COX-1 inhibitors), and Polyunsaturated Fatty Acids (Omega-3 Fatty Acids) have demonstrated effectiveness – sometimes surpassing first-line psychotropic medications – in reducing psychiatric symptomatology.
It has also been demonstrated that some antidepressant and antipsychotic medications exert measurable immune modulation and anti-inflammatory effects. This may in part explain some of their therapeutic actions further challenging the theoretical foundation of the neurotransmitter hypothesis.
The notion of neuroinflammation is opening the door to a groundbreaking scientific endeavor. There is even a debate among these trailblazing scientists about what to call this promising and emerging field; Immunopsychiatry or Psychoneuroimmunology.
A conspicuous question is then raised as to whether inflammation causes mental impairment or does psychiatric pathology induce inflammation? Is inflammation the chicken or the egg? This is an exciting new frontier in psychiatry. It will offer promising novel targets for treatment and new avenues for therapeutic innovation.