Myelolipoma of the kidney: A review and update
Received: 19-Feb-2018 Accepted Date: Mar 05, 2018; Published: 12-Mar-2018
Citation: Venyo AKG. Myelolipoma of the kidney: A review and update. J Kidney Treat Diagn. 2018;1(1):8-15.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
Less than 10 cases of myelolipoma have been reported in the kidney as well as around the kidney. Myelolipoma involving the kidney, perirenal tissue or renal sinus may be discovered incidentally as part of investigation of other diseases; the disease may also present with loin pain, abdominal pain, abdominal bloating, haematuria or other non-specific symptoms. Radiological imaging tends to show a kidney mass with fat density attenuation on CT or MRI scan which tends to be non-contrast enhancing or it may show minimal enhancement. Diagnosis tends to be established by pathology finding of adipose tissue admixed with normal haematopoietic cells including all the three haematopoietic cell lineages (granulocytic, erythroid, as well as megakaryocytic). The disease may coexist with other diseases. The disease which exhibits a benign biological behaviour has been associated with various management options including conservative/surveillance approach, partial nephrectomy, radical nephrectomy or by complete excision of lesions surrounding the kidney whilst preserving the kidney. The lesion may derive its blood supply circumferentially from a peripheral leash of vessels and that there the lesion may not have a single arterial supply embolization may perhaps not be feasible in some cases. Differential diagnoses of the disease include: sarcomas of the kidney including liposarcoma, renal cell carcinoma, angiomyolipoma, and transitional cell carcinoma of the renal pelvis involving the renal parenchyma. The ensuing concluding summations would be made based upon the available literature on myelolipoma of the kidney: Myelolipoma is a rare benign disease and if it is diagnosed by undertaking radiological imaging guided biopsies/aspiration cytology a number of cases that a diagnosed in the future, it could be managed conservatively using the radiological imaging surveillance approach and the partial/radical nephrectomy option could be reserved for very large or symptomatic lesions.
Keywords
Myelolipoma, Kidney, Adipose tissue, Fat, Haematopoietic cells, Nephrectomy, Granulocytic, Erythroid, Megakaryocytic.
Introduction
On day to day basis a number of lesions tend to be encountered in kidneys based upon various radiological imaging techniques which need to be investigated to establish the actual cause and when malignancies of the kidneys are encountered and found to be localized a large number of patients tend to undergo surgical operations in the form of radical nephrectomy or partial nephrectomy depending upon the size and position of the tumour and the co-morbidities of the patients as treatment options of curative intent. Other treatment options for some renal tumours include active surveillance, radiofrequency ablation of small renal tumours, cryotherapy of small tumours, and electroporation of renal tumours. Many other renal masses exist including angiomyolipoma, oncocytoma, myelolipoma, glomangiomyoma and other lesions. Difficulties do exist with regard to deciding whether or not a renal tumour is benign and when both the radiologist and the urologist are sure that a renal lesion is benign such a tumour tends to be left alone without surgery but in situations where the exact diagnosis is not certain or situations where the risk of spontaneous bleeding with procedure options including partial nephrectomy, radical nephrectomy or selective renal angiography and super-selective embolization of the artery feeding the renal lesion. Myelolipoma does occur in various organs and most commonly these have been reported in the adrenal gland. To the knowledge of the author, only four cases of myelolipoma of the kidney have been reported in the global literature in view of this it is envisaged that majority of clinicians would be unfamiliar with the clinical features and management of myelolipoma of the kidney. If clinicians are aware that a kidney lesion is benign and as well as it is a myelolipoma they would most likely not consider surgical operation in majority of the cases they encounter. The ensuing document related to myelolipoma of the kidney is divided into two parts: (A) Overview and (B) miscellaneous narrations from reported cases.
Myelolipoma of the kidney is a very rare benign disease which may mimic other renal lesions which majority of clinicians may be unaware of.
Aim
To review the literature on myelolipoma of the kidney
Methods
Various internet data bases were searched including: Google, Google Scholar, PUB MED, and Educus. The key words used included myelolipoma of the kidney and renal myelolipoma.
Review of Literature
Overview of Myelolipoma of the kidney
General comment and definition: Myelolipomas are benign lesions that tend to comprise of (adipose tissue) and haematopoietic elements and usually have been commonly reported in the adrenal gland in comparison with in other organs [1].
Epidemiology: The following summations have been made in relation to myelolipoma of the kidney:
a. Myelolipoma of the kidney is rare.
b. Fewer than 50 cases of myelolipoma have been reported that have been located outside the adrenal gland and fewer than 25 cases of myelolipomas have been reported associated/located in the kidney.
c. Myelolipoma of the kidney may be found contemporaneously with other tumours for example papillary urothelial carcinoma as reported by Greaves and associates [2].
Pathophysiology: It has been intimated that the pathogenesis of myelolipoma is not clear or not well understood. [3,4]. Nevertheless, the ensuing postulates exist: It had been stated that majority of the postulations have involved the development as well as differentiation of either ectopic adrenal rests or haematopoietic stem cell rests in response to triggering effects of a stimulus, especially endocrine dysfunction Bishop et al. [5,6] did find clonal cytogenetic abnormalities, which in their opinion had indicated that myelolipoma was of tumour origin.
It had been iterated that chromosomal translocations that had been identified within myelolipomas and in benign lipomatours neoplasms that are seen in relation to acute myelogenous leukaemia or myelodysplastic syndrome would suggest that the origin of myelolipoma to be bone marrow, and this could indicate that myelolipoma would tend to be derived from erroneously transferred erythroid cells. [7].
Presentation: a. Myelolipoma may be asymptomatic and this may be diagnosed incidentally based upon radiological imaging for a different condition based upon ultrasound scan, computed tomography scan or magnetic resonance imaging scan.
b. Myelolipoma of the kidney could perhaps present with loin pain.
c. Myelolipoma could present with haematuria.
Clinical features: Considering that myelolipoma of the kidney is a benign lesion it wold tend to exhibit a benign biology behaviour.
1. Haematology investigations-Full blood count and coagulation screen would tend to be undertaken in the general assessment of a patient with myelolipoma of the kidney; but the results would not be diagnostic of myelolipoma of the kidney.
2. Biochemistry investigations-Serum urea and electrolytes, liver function tests, and serum glucose would tend to be undertaken in the general assessment of a patient with myelolipoma of the kidney but none of the results would be diagnostic of myelolipoma of the kidney.
3. Microbiology investigations-Urine analysis, microscopy and culture would tend to be undertaken as part of the general assessment of a patient with myelolipoma of the kidney; but the results would not be diagnostic of myelolipoma of the kidney.
Radiological investigations
1. Ultrasound scan: Ultrasound scan of renal tract or ultrasound of abdomen and pelvis would show a lesion within or around the kidney that would alert the clinician to investigate and establish the cause of the lesion; it also enables the site and size of the lesion to be measured as well as ultrasound scan guided aspiration cytology or biopsy of the lesion to be undertaken to establish the diagnosis as well as ultrasound scan of renal tract can be undertaken in the follow-up of patients undergoing conservative management/surveillance or follow-up pursuant to undergoing surgical treatment. If contrast enhanced ultrasound scan (CEUS) is undertaken this would tend to show non-contrast enhanced lesions which would tend to be around the renal hilum. The lesion could be found around the renal hilum or the peripheral aspect of the kidney.
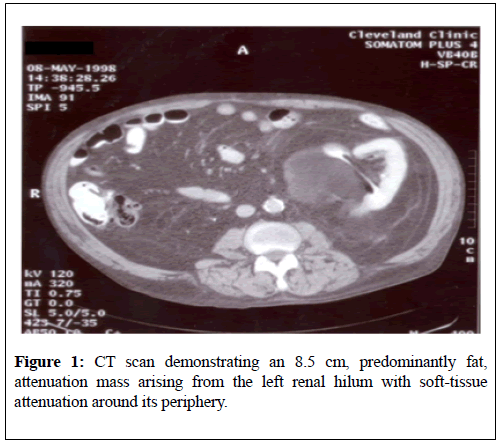
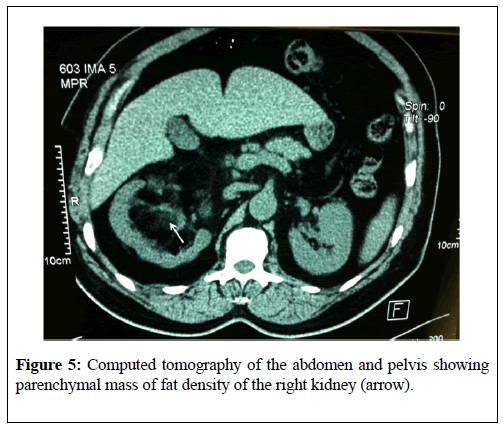
2. Computed tomography scan: Computed tomography (CT) scan is a useful radiology imaging option for the investigation and diagnosis of myelolipoma of the kidney. CT scan of abdomen and pelvis would tend to show a solid mass in the kidney with fat density attenuation (less than 20 Hounsfield units) and they also tend to be non-contrast enhancing as well as the lesions may tend be found near the hilum or peripheral aspect of the kidney and the lesions may also be found around the ureter or within the kidney tissue. There would tend not to be calcification/ossification associated with the lesion. If there are any associated lesions within the kidney or elsewhere in the abdomen and pelvis the CT scan would also show it.
CT scan-guided aspiration cytology/CT guided biopsy of the kidney lesion can be taken for pathology examination which would then reveal fat tissue lesion admixed with haematopoietic tissue and no malignant cells. CT scan of abdomen and pelvis can be used to monitor of the progress of a small myelolipoma that is being managed conservatively or expectantly by surveillance periodically.
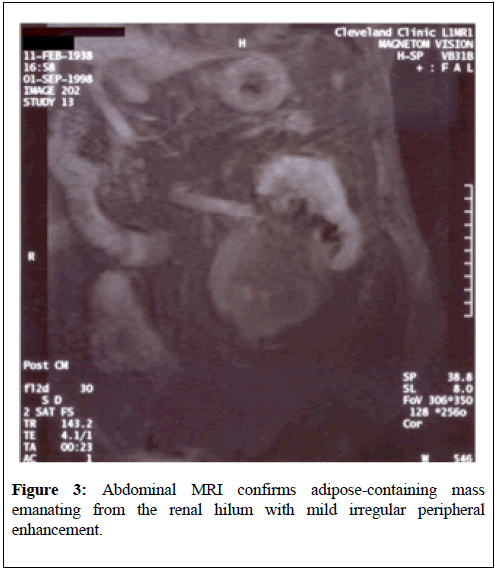
3. Magnetic Resonance Imaging (MRI) scan: a. Magnetic Resonance Imaging (MRI) scan is a useful radiology imaging option for the investigation and diagnosis of myelolipoma of the kidney. MRI scan of abdomen and pelvis would tend to show a solid mass in the kidney with fat density attenuation (less than 20 Hounsfield Unit) and if there are any associated lesions within the kidney or elsewhere in the abdomen and pelvis the MRI scan would also show it. These fat density lesions may be found in the renal hilum or periphery of the kidney and most often because they are benign lesions they would tend to be non-contrast enhancing and they would tend not to be associated with calcifications/ ossifications The lesions could be found in the renal hilum, within the kidney tissue, around the ureter or peripherally on the kidney.
b. MRI scan-guided aspiration cytology/MRI guided biopsy of the kidney lesion can be taken for pathology examination which would then reveal fat tissue lesion admixed with haematopoietic tissue and no malignant cells.
c. MRI scan of abdomen and pelvis can be used to monitor of the progress of a small myelolipoma that is being managed conservatively or expectantly by surveillance periodically. The advantage of MRI scan of abdomen and pelvis in the monitoring of patients on surveillance of their myelolipoma of the kidney is that there would not be any cumulative radiation effect on the patient over many years.
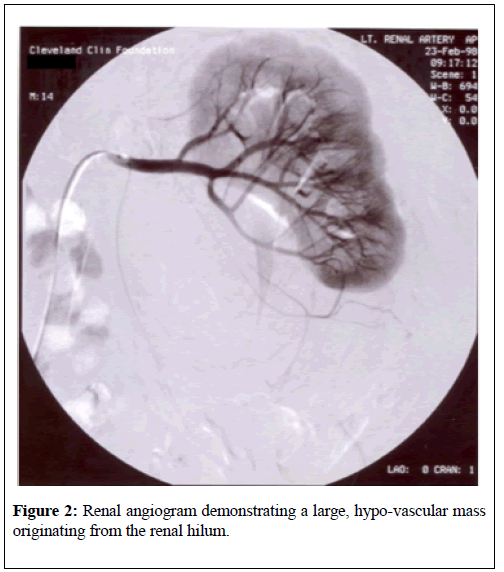
4. Selective renal artery angiography: Renal artery angiography is an interventional radiology investigation that can be used to assess the blood supply of the myelolipoma of the kidney as it can also be used to assess the blood supply of renal malignancies as well as angiomyolipoma of the kidney. Considering that renal malignancies and angiomyolipoma of the kidney tend to have arterial blood supply to the lesions they can be selectively embolized; nevertheless, since myelolipomas of the kidney tend to have fat tissue admixed with haematopoietic lineage cells they would most likely be fed by peripheral leash of vessels without a main feeding artery that could be embolized as a treatment option. One cannot be certain with regards to the blood supply to myelolipomas of the kidney but with time when more cases are reported furthermore lessons would be learnt with regards to the arterial blood supply of myelolipoma of the kidney.
Treatment options used
Some of the treatment options for myelolipoma of the kidney include:
1. Conservative management of small lesions as well as asymptomatic lesions.
2. Partial nephrectomy (Open or laparoscopy technique).
3. Radical Nephrectomy (Open or laparoscopy technique).
4. Total excision of myelolipomas encompassing the kidney and ureter without involving the kidney tissue or ureter.
5. Selective angiography and embolization of the arterial supply to the lesion may not be possible because there may not be a single blood supply to the lesion.
Pathology findings
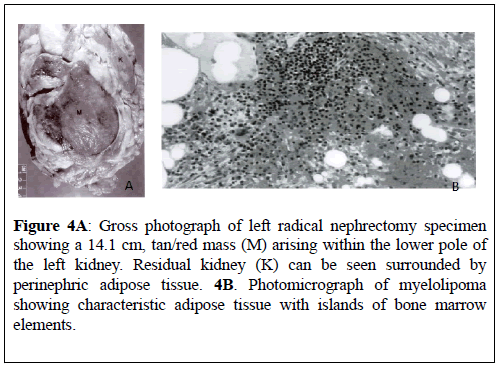
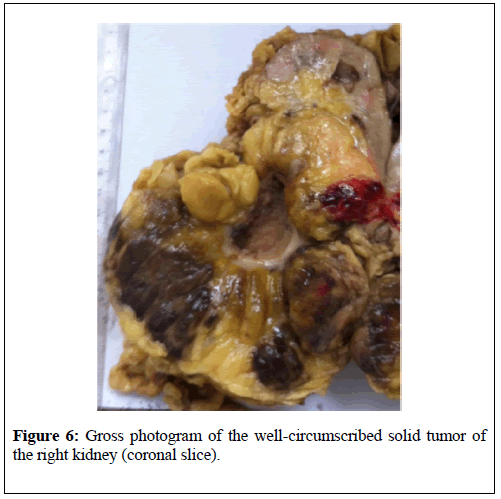
a. Macroscopic features- Gross examination of a myelolipoma may reveal a well-circumscribed, non-encapsulated, solid mass in the kidney. The cut surface of myelolipoma would tend to reveal areas of soft yellow fatty tissue together with admixed with irregular areas of brownish friable tissue [4ghaouti].
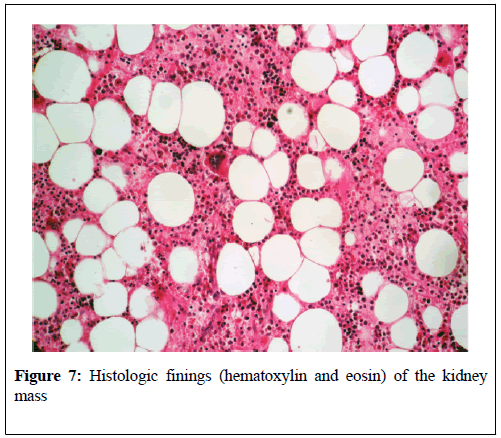
b. Microscopic features- The typical histological examination findings on pathological examination of specimens of myelolipoma of the kidney have been summated as follows:
• A mixture of adipose (fat) tissue and normal haematopoietic cells tend to be seen on microscopy.
• No evidence of bony spicules tends to be seen on microscopic examination of specimens of myelolipoma of the kidney.
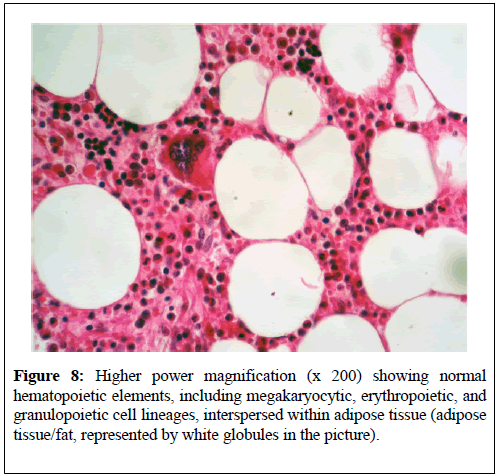
• Microscopic examination tends to show all the three haematopoietic cell lineages (granulocytic, erythroid, as well as megakaryocytic). With regards to definition, there tends not to be any connection of myelolipoma of the kidney to medullary cavity of any bone.
• It may co-exist with other renal lesions or tumours in that case the histology features of the additional lesion or lesions may be seen but these features would not diagnose myelolipoma.
Differential diagnoses
Some of the differential diagnoses of myelolipoma of the kidney include:
• Angiomyolipoma
• Lipomatosis
• Sarcoma including liposarcoma
• Transitional cell carcinoma
• Renal cell carcinoma
• Metastatic tumours
Treatment
When diagnosis of myelolipoma of the kidney is established depending upon the size and size of the lesion and depending upon whether, or not the patient is symptomatic the following treatment options can be used:
• Conservative treatment with radiological imaging surveillance
• Partial Nephrectomy (open or laparoscopic approach)
• Radical Nephrectomy (open or laparoscopic approach)
• Excision of the lesion if it is surrounding the kidney/ureter but not involving them
Outcome
• Myelolipoma of the kidney is a benign tumour that is associated with good prognosis
Miscellaneous Narrations from Some Reported Cases and Discussions
Myelolipoma was first described in 1905 by Gierke [8] since then myelolipomas have been reported sporadically in various organs but most commonly they have been reported in the adrenal gland. It had been documented that the finding of myelolipomas in extra-adrenal sites tends to be uncommon and that an incidence of the occurrence of extra-adrenal myelolipoma had been documented to be 0.4% in autopsy specimens [4-9].
Extra-adrenal myelolipoma have been stated to have been reported in the retroperitoneum, pelvis, pre-sacral area, thorax, mediastinum, stomach, liver, and the thyroid gland [10].
Beraha et al. [11] in 1974 reported a 64-year-old man who had arteriography to investigate his peripheral vascular disease which incidentally revealed a left renal mass. The results of his full blood count and his routine blood biochemistry tests were normal. He had excretory urography which revealed a left mass which had displaced the left kidney cephalad and which had displaced the left ureter medially. He underwent left nephrectomy on 16th November 1972. Macroscopic examination showed that the tumour had measured 13 cm × 13 cm × 10 cm and it was an encapsulated, firm yellow mass that was attached to the perirenal fat with fibrous adhesions. The tumour was noted to have compressed but did not arise from the parenchyma of the kidney. Microscopic examination of the tumour showed mainly mature adipose tissue with numerous islands of brownish tissue that comprised of hematopoietic cells that mimicked those found in bone marrow and the pathological features of the tumour was adjudged to be consistent with myelolipoma.
Xuefeng and Minglu [10] reported a 44-year-old man who was admitted because of dystrophy of his right kidney and renal calculus. He did have ultrasound scan of renal tract which showed right hydronephrosis. He also had intravenous urogram which showed that the contour of the right kidney was un-clear, and there was evidence of a circular high-density shadow inside the kidney. He underwent right nephrectomy and the pathology examination findings were adjudged to be consistent with myelolipoma of the right kidney.
Clarke et al. [12] reported a 59-year-old Caucasian man who presented left loin and left upper abdominal pain of pain of 4 months duration which was associated with fullness of the abdomen, worsening wheezing, dyspnoea on exertion, poor appetite, and 20 pounds weight loss. He did not have any lower urinary tract symptoms or haematuria. His past medical history included: sarcoidosis of 33 years duration for which he was on long-term steroids, chronic obstructive pulmonary disease, type 2 diabetes mellitus, hypertension, gout, coronary artery disease, morbid obesity and phrenic nerve paresis. He was found on examination to have mild tenderness and fullness in the left upper abdomen. The results of his haematology and routine biochemistry blood tests were normal. He had computed tomography scan of abdomen which showed an 8.5 cm left renal hilum mass which had fat attenuation which was adjudged to be consistent with angiomyolipoma (Figure 1).
Considering the patient’s comorbidities interventional radiological selective left renal artery angiography and super-selective embolization of the mass was attempted. He had left renal artery angiography which showed a large relatively hypo-vascular, mass that projected from the lower pole of the left kidney (Figure 2).
The only vascularity that was present arose from small renal and cortical branches that remained at the periphery of the mass. There was no evidence of any single arterial supply to the mass that was conducive for embolization therefore the embolization procedure was abandoned. It was therefore decided to monitor the progress of the mass by means of serial radiological imaging monitoring a computed tomography scan of abdomen and pelvis was undertaken 5 months subsequently and this showed a left-sided 9.0 cm mass with fat attenuation which was felt was retroperitoneal rather than a hilar mass.
A renogram was undertaken at that time which did show normal arterial flow and the differential renal function was right kidney 55%, and left kidney 45%. The patient was offered surgical excision of the mass because of the increase in size; however, he did not accept the offer of surgical operation at that time, but he asked for the procedure to be delayed until the next summer. Ten months after his initial presentation he had magnetic resonance imaging scan of his abdomen and pelvis which showed a 9.2 cm left sided mass with the epicentre in the left renal sinus and apparently confined to the Gerota’s fascia (Figure 3).
The T2 signal intensity was adjudged to be consistent with fat and the left renal vein was found to be patent. He underwent exploration off the mass through an anterior trans-abdominal approach and during the procedure a large left renal mass was found for which left radical nephrectomy was performed. He made a good post-operative discovery and was discharged on the 8th post-operative day. Gross examination of the specimen showed a 14.1 cm × 10.2 cm × 6.8 cm mass which had replaced the lower pole of the left kidney and which did appear to have originated in the renal sinus.
The mass was observed to be grossly circumscribed and demarcated sharply from the encompassing parenchyma of the kidney, but it was unencapsulated (Figure 4A). Gross examination of the cut section of the specimen the mass was found to be yellow-red, which had an oily surface. Areas of recent haemorrhage were identified but there was no evidence of necrosis. Histology examination with microscopy of the specimen showed areas of mature adipose tissue and haematopoiesis which was consistent with myelolipoma that had originated in the left kidney (Figure 4B). Immunohistochemistry studies of the adipose areas were negative for HMB–45 and smooth muscle actin. There was no evidence of an adrenal rest in the specimen. Histology of the adrenal gland was normal. A final diagnosis of myelolipoma of the left kidney was made.
Figure 4A: Gross photograph of left radical nephrectomy specimen showing a 14.1 cm, tan/red mass (M) arising within the lower pole of the left kidney. Residual kidney (K) can be seen surrounded by perinephric adipose tissue. 4B. Photomicrograph of myelolipoma showing characteristic adipose tissue with islands of bone marrow elements.
Greaves et al. [2] reported a 64-year-old man who had a unique case of myelolipoma of the renal sinus that presented as a mass which had coexisted with papillary transitional cell carcinoma. This 64-year-old man with a history of transitional cell carcinoma of the urinary bladder who presented with visible haematuria and a filling defect in the renal pelvis which was demonstrated on computed tomography scan. Pathology examination of the specimen showed an irregular fatty myxoid mass as well as high-grade papillary transitional cell carcinoma. The differential diagnoses that were considered did include: myxoid liposarcoma, myxoid variant of malignant fibrous histiocytoma (myxoid fibrosarcoma), and angiomyolipoma. Immunoperoxidase staining of the specimen did confirm presence of hematopoietic cells and furthermore, diagnostic histology features and immunohistochemistry features of liposarcoma, myxofibrosarcoma, and angiomyolipoma were not demonstrated. Based upon the histology features and the immunohistochemistry characteristics of the tumour, it was adjudged that the lesions were myelolipoma and transitional cell carcinoma which had appeared to be unrelated co-existent entities.
Brietta et al. [13] reported a 66-year-old diabetic woman who had an extremely large perirenal giant extra-adrenal myelolipoma.
Amin et al. [14] reported a 66-year-old man who had a history of bipolar manic-depressive disorder for the preceding 15 years which had been treated by means of lithium carbonate who was admitted because of abdominal pains and recurrent urinary tract infections. His haematology tests revealed mild normocytic normochromic anaemia and mild leucocytosis and his blood biochemistry tests were normal. His urine culture grew Escherichia coli. He had computed tomography scan which had shown a 5.5 cm mass which was adjudged to be possibly emanating from the left renal sinus and evidence of splaying of the collecting system. The CT scan of the abdomen did not show any other abnormality. Based upon the CT scan features of the mass the differential diagnoses that made provisionally included sarcoma (possibly liposarcoma), transitional cell carcinoma, renal cell carcinoma, and metastasis. However, the most likely provisional diagnosis of sarcoma was made. A CT-guided aspiration of the specimen of the specimen was undertaken for cytology examination and the features of the specimen were adjudged to be consistent with myelolipoma. He underwent left radical nephrectomy and after a followup of 62 months there has not been any recurrence of his lesion and he had not had any problems related to the left renal lesion. Macroscopic examination of the radical nephrectomy specimen showed that the renal sinus had contained a 7.5 cm × 3 cm × 2.8 cm soft mass lesion that was red-brown in colour and which also had focal yellow areas and fine granular cut surface. The lesion was found to be partially encapsulated; however, the lesion appeared to creep into the hilar fat in the anterior aspect in a serpiginous fashion. The mass had abutted and encompassed the pelvicalyceal system; nevertheless, the mass did not involve the mucosa. The renal parenchyma was not involved by the tumour mass. The pelvicalyceal system was mildly dilated, and the mucosa did have a dull, greyish-white, finely granular appearance. The parenchyma of the kidney was grossly unremarkable, and it did have a sharp cortico-medullary distinction. Microscopic examination of the specimen depicted characteristic features of myelolipoma that comprised of a mixture of an admixture of mature adipose tissue and hematopoietic cells that varied in proportions one area to another area. There was evidence of cells from the 3 hematopoietic cell lines inclusive of myeloid, erythroid, and megakaryocytes. The myeloid/erythroid cell ratio, as was computed from the previous fine-needle aspiration material 2.5/1. Various small lymphoid aggregates, some of which did have ill-defined germinal centres, and which were admixed with plasma cells were observed both in close approximation and away from the hematopoietic elements. On microscopic examination it was also observed on microscopic examination that the hematopoietic foci had been associated with haemorrhagic background but contrarily, there was a relatively clean nonhaemorrhagic background observed within areas of the inflammatory cell aggregates. Within the haemorrhagic areas, scattered hemosiderin-laden macrophages were observed as well as there was no evidence of any bony trabeculae were observed anywhere within the lesion. The parenchyma of the kidney looked normal and was not involved as well as the pelvicalyceal system was not involved by the lesion. Dense lymphoplasmacytic infiltration with focal germinal centre formation and fibrosis of the walls was observed. The adrenal gland looked normal.
Ghaouti et al. [4] reported a 55-year old Moroccan male who was known to have insulin dependent diabetes mellitus who did present with right loin pain. His general and systematic examinations were normal. The results of his serum biochemistry and his haematology blood tests were all normal. He had ultrasound scan of his renal tract which did show right hydronephrosis. He did undergo retrograde ureteropyelogram studies and the left retrograde radiological studies did show hydronephrosis which had been caused by calyceal and pelvic lithiasis and a non-functioning right kidney. He additionally had computed tomography scan of abdomen and pelvis which did reveal a relatively well-circumscribed parenchymal mass of fat-density that measured 10 cm in diameter which did not involve the peri-nephric fat (Figure 5). His adrenal glands were seen to be normal and no abnormal lymph node enlargements were seen on the CT scan. A laparotomy and right nephrectomy was undertaken with removal of the hydronephrotic kidney. Macroscopic examination of the specimen revealed an irregularly shaped right kidney that weighed 800 grams, and which did measure 15 cm × 11 cm × 8 cm and on the lower pole of the kidney was found a relatively well- circumscribed, non-encapsulated solid mass that had measured 11 cm × 8 cm × 8 cm. Macroscopic examination of the cut surface of the lesion did show areas of soft tallow fatty (adipose) tissue that was admixed with irregular areas of brownish friable tissue (Figure 6). Microscopic examination of specimens of the renal lesion showed that the tumour had comprised of mature adipose (fat) tissue as well as nests of haematopoietic precursor cells that mimicked those found within normal bone marrow (Figure 7). Furthermore, there was evidence of all the three haematopoietic cell lineages including granulocytic, erythroid, and megakaryocytic cells (Figure 8). There was evidence of scattered small lymphoid aggregates as well as foci of haemorrhage but there was no evidence of adrenal rests within the specimen. As part of further investigation to establish a definite diagnosis he had bone marrow aspiration and histological examination revealed normocellular based upon the pathology findings a diagnosis of myelolipoma of the right kidney was established. He had an uneventful post-operative recovery and was well and disease free at his 3-month follow-up. Ghaouti et al. [4] stated the following:
Figure 6: Gross photogram of the well-circumscribed solid tumor of the right kidney (coronal slice).
Figure 8: Higher power magnification (x 200) showing normal hematopoietic elements, including megakaryocytic, erythropoietic, and granulopoietic cell lineages, interspersed within adipose tissue (adipose tissue/fat, represented by white globules in the picture).
At the time of their case report in 2013, only six cases of myelolipomas that arose around the peri-renal tissue had been reported globally [3] and only two cases of myelolipoma involving the parenchyma of the kidney had been reported in the global literature [10,11].
Their reported case was the third case of myelolipoma involving the parenchyma of the kidney to be reported in the world literature.
Talwalker et al. [3] reported a 65-year-old Caucasian man who had presented with loin pain, haematuria, dysuria and weight loss. His previous medical history did include diabetes mellitus, chronic obstructive pulmonary disease, hypertension, atresia of large bowel, hypercholesterolemia, and osteoporosis which had been complicated by fracture of the vertebra. He had thoracic X-ray, computed tomography scan of thorax, abdomen and pelvis which showed a suspicious nodule in the right middle lobe of the lung, a 0.5 cm ring-enhancing mass which was an arteriovenous malformation in the lingular segment of the upper lobe of the left lung, a non-enhancing homogenous low-attenuation mass which measured 5.5 cm × 4.5 cm that appeared to have arisen from the right renal pelvis and located anterio-medial to the right kidney. Based upon the CT scan findings the differential diagnoses that were considered included renal cell carcinoma and transitional cell carcinoma that had involved the renal parenchyma. He also had intravenous pyelogram which did show that the lesion was extra-renal with regards to location. He underwent right nephrectomy and did recover well from the operation. Macroscopic examination showed that the right including the mass had weighed 650 grams and that the mass was spheroid, well-circumscribed, and adherent to the anteromedial surface of the lower half of the right kidney and the mass had measured 7 cm × 5 cm × 1.5 cm. The cut surface of the mass was found to be relatively flat, glistening, and tan to mostly mahoganypink, associated with irregularly scattered punctate red markings as well as delicate stellate grey streaks that radiated centrifugally away from the centre. Microscopic examination of the specimen revealed the following features:
• The specimen was comprised of mostly adipose (fat) tissue together with multiple scattered islands of haematopoietic precursor cells.
• The cellularity of the haematopoietic precursors did vary.
• The three haematopoietic cell lineages including granulocytic, erythroid, and megakaryocytic types were all seen.
• There was presence of small lymphoid aggregates were scattered and some of the lymphoid aggregates had demonstrated ill-defined germinal centres that had been mixed with plasma cells that were observed to be in close approximation to as well as distant from the haematopoietic elements.
• Both the haematopoietic cellular sites and the lymphoid aggregates were linked haemorrhage and hemosiderin-laden macrophages.
• There was no evidence of any bony trabeculae.
• The adjacent adrenal gland was normal.
A diagnosis of myelolipoma arising adjacent to the renal hilum was made. No adenopathy was identified.
The tumor is composed of mature adipose tissue and islands of hematopoietic elements with intermingled megakaryocytes (original magnification x 100) Fat cells showing as white globules.
Cox et al. [15] reported a 62-year-old woman who had bilateral extraadrenal myelolipoma who had many co-morbidities that presented with vague abdominal pain. She had investigations including cystoscopy and left retrograde retro-grade ureteropyelogram, computed tomography scan of abdomen and pelvis, magnetic resonance imaging scan of abdomen and pelvis as well as CT scan guided biopsy of left renal sinus mass and histology examination of the specimen showed adipose tissue, hemosiderin and hematopoietic element. She had normal bone marrow assessment and as well as molecular biology assays which did not reveal anything to confirm the diagnosis. Diagnosis of myelolipoma was established based upon histological examination of specimens from left nephrectomy and excised retroperitoneal mass.
Iflazoglu et al. [16] reported a 26-year-old woman with no significant past medical history who presented with abdominal pain and malaise. She had ultrasound scan of abdomen and pelvis as well as computed tomography scan of abdomen and pelvis which showed an 8cm right perirenal mass not related to the adrenal gland. The results of her laboratory investigations showed she had iron deficiency anaemia and vitamin B12 deficiency. Her haemoglobin was 6.2 grams/decilitre; her white blood cell and platelet counts were within normal range; Her C-reactive proteins and ferritin tests were undertaken, and the indirect Coombs test was stated to be positive. Her blood and urine cultures were negative. Her Brucella and salmonella serology tests were negative. Her tumour levels of CA 125, CA 19-9, and CEA were normal. During her admission her haemoglobin dropped to 3.8 grams/decilitre. Her peripheral blood smear results were consistent with partial haemolysis. She was empirically started on antibiotic combination treatment with ceftriazone 2 grams and metronidazole 1.5 grams daily. The results of her bone marrow aspiration and smear examinations indicated she had haemolytic anaemia. She has intravenous prednisolone and blood transfusion. She was also treated with oral deltacortril 10 mg per day and her haematological parameters had stabilized. She undergone insertion of right ureteric stent and surgical exploration which did reveal the ‘8 cm mass’, encompassing the right ureter which had a thin wall. The mass was completely excised successfully and the right ureter, right kidney as well as right adrenal gland were preserved and left intact. Her deltacortril medication was continued in decreasing doses and the medication was stopped on the 20th post-operative day. She had continued to do well and at her follow-up her haematological profile was stable. Macroscopic examination showed that the mass had measured 8 cm x 6 cm x 6 cm and it had an intact capsule. The external appearance of the mass was partly yellow and partly brown. Microscopic examination of the specimen showed fat cells and dispersed among the fat cells were non-uniform haematopoietic areas that contained granulocytic, erythrocytic, and megakaryocytic elements. The pathology features of the mass were adjudged to be consistent with myelolipoma.
With regards to radiological diagnosis of myelolipoma there are no specific radiological imaging features that have been agreed upon to clearly diagnose myelolipoma of the kidney and clearly differentiate it from the differential diagnoses. Histological examination of biopsy specimen; one of the differential diagnoses of myelolipoma of the kidney. The cornerstone for the diagnosis of angiomyolipoma of the kidney based upon all radiological imaging modalities tends to be the demonstration of macroscopic fat; nevertheless, in the scenario of intra-renal haemorrhage or when the angiomyolipoma lesions do contain little fat, it could prove difficult to differentiate angiomyolipoma from renal cell carcinoma [17] and from myelolipoma. With regards to angiomyolipoma of the kidney ultrasound scan rends to show hyper-echoic lesions which tend to be located within the cortex of the kidney with posterior acoustic shadowing and contrast enhanced ultrasound scan tends to show enhancement peripherally as well as decreased central enhancement in comparison with normal cortex of the kidney. CT scan in cases of angiomyolipoma of the kidney tend to show fat density lesions mostly in the cortex with a density of less than 20 Hounsfield Units (HU) but when the angiomyolipoma contains little fat it tends to be difficult to differentiate it from a small renal cyst. MRI scan of the kidney in angiomyolipoma of the kidney tends to show (a) high signal intensity on non-fat-saturated sequences and loss of signal following fat saturation and (b) out of phase imaging which generates India Ink Artefact at the interface between fat and non-fat components either at the interface between the angiomyolipoma and the surrounding kidney or between fat and non-fat component of the mass. [17,18] Nevertheless, considering that rarely renal cell carcinoma could on rare occasions presence of fat in a renal mass should not automatically be diagnosed as angiomyolipoma of kidney for certain. Furthermore, in angiomyolipoma of the kidney in addition to the fat density lesions of less than 20 Hounsfield unit (HU) on CT and MRI scans, there tends to be imaging evidence of the vascular component (obvious vessels) which tend to be absent in myelolipoma of kidney. It is worth noting that macroscopic fat in renal cell carcinoma almost invariably tends to occur in the presence of calcification/ossification, therefore when there is absence of ossification or calcification then the lesion could be considered angiomyolipoma. Liposarcoma of the kidney may be found in the peripheral aspect of the kidney and ultrasound scan, CT scan and MRI scan may show evidence of contrast enhanced lesion in the periphery or lateral border of the kidney with calcification [19] Because of some fat tissue within the lesion there may be areas of low-fat intensity on contrast enhanced images depending upon the size of the fatty component but the sarcomatous areas could yield areas of contrast-enhancement but these would not specifically diagnose the disease therefore histological examination of biopsy specimen or the nephrectomy specimen would tend to confirm the diagnosis.
Urothelial carcinoma or transitional cell carcinoma of renal pelvis may extend into the renal tissue with regards to invasive cases, but these tend to be associated with filling defects within the renal pelvis in majority of cases and the diagnosis could be established by doing urine cytology and ureterorenoscopy and biopsy of the lesion within the renal pelvis.
Other types of renal malignant renal tumours including renal cell carcinoma and sarcomas would tend to be seen on CT scan or MRI scan as contrast enhancing lesions. Additionally utilization of radiological imaging (CT scan or MRI scan) of thorax, abdomen and pelvis would confirm there is no other lesion and elsewhere and therefore the lesion in the kidney is not a metastatic malignant lesion and furthermore the benign features of the lesion on histological examination would confirm the lesion is benign which would reassure the patient.
Summary
Myelolipoma of the kidney is a rare benign tumour which consists of adipose tissue and haematopoietic elements. Myelolipoma may be encountered in the male as well as in female whose ages have tended to range between 40 years and 80 years; however, majority of the few reported cases of myelolipoma of the kidney have been reported in individuals in their seventh decade of life.
Myelolipoma of the kidney may be diagnosed as an incidental finding of a renal mass on radiological imaging as part of investigation for another disease especially in cases of small myelolipomas of the kidney. Large myelolipomas of the kidney may present with loin pain, vague upper abdominal pain/discomfort, abdominal fullness/abdominal bloated-ness, haematuria and or other constitutional symptoms. Myelolipoma of the kidney may be found in association with other renal diseases including calculi or other types of renal tumours. Myelolipomas of the kidney may also be found in association with other extra-renal lesions. The lesions could be within the kidney, the renal sinus or encompassing the kidney and ureter.
Diagnosis of myelolipoma of the kidney may be suspected by the finding of a radiological imaging evidence of a renal lesion with fat density (less than 20 Hounsfield Units) with usually no evidence of contrastenhancement and no ossification/calcification associated with the lesion.
Diagnosis of myelolipoma of the kidney may be made upon histology examination of specimens of the renal lesions showing adipose (fat) tissue and haematopoietic elements and absence of malignant cells in specimens obtained by (a) aspiration cytology, (b) radiological imaging-guided core biopsies of the renal lesion, (c) biopsies of the renal lesion taken via the laparoscopic approach, partial nephrectomy specimens containing the lesion, or radical nephrectomy specimens containing the tumour.
Myelolipomas of the kidney may be managed as follows
• Conservative management of small asymptomatic lesions
• Partial Nephrectomy (open or laparoscopic approach)
• Radical Nephrectomy (open or laparoscopic approach)
• Complete excision of the lesion when it is encompassing the kidney/ ureter in cases of peri-renal myelolipomas not really involving the renal tissue.
Selective renal artery angiography and super-selective embolization of the branch of renal artery supplying the lesion may be considered; nevertheless, an anecdotal report has shown that renal artery angiography may demonstrate that there is no single main artery supplying the myelolipoma of the kidney and that the lesion is being supplied by a leash of vessels encompassing the myelolipoma and hence embolization of the myelolipoma of the kidney may not be feasible.
Myelolipoma of the kidney tends to exhibit a benign biological behaviour and tends to be associated with good prognosis following surgical treatment but small lesions can be treated conservatively by surveillance and with periodic radiological imaging in asymptomatic- patients but large lesions and lesions associated with symptoms should be managed by partial nephrectomy or radical nephrectomy depending upon the site and size of the lesion.
CONCLUSION
Myelolipoma of the kidney is a rare benign tumour that is associated with good prognosis. The lesion is diagnosed by the finding of a renal lesion with fat density and upon histology finding of fat tissue and haematopoietic elements in the lesion as well as absence of malignant cells. Because of the rarity of the lesions clinicians should be encouraged to report cases of myelolipoma of the kidney they encounter, so as to further elucidate the biological behaviour of the disease.
Acknowledgement
Acknowledgements to Hindawi Publishing Journals publishing cooperation and Scientific World Journal as well as BioMed Central for granting copy right permission for figures and contents of their articles to be reproduced under Creative Commons Attribution License.
REFERENCES
- Ziadie M. Kidney tumor–cysts, children, adult Benign (usually) adult tumors. Myelolipoma. Pathology Outlines. 2017.
- Greaves WO, Khanna P, DeLellis R, et al. Renal sinus myelolipomacoexistent with renal pelvis papillary transitional cell carcinoma: a case report. Int J Surg Pathol. 2010;18(5):437-39.
- Taiwalker SS, Shaheen SP. Extra-adrenal Myelolipoma in the Renal Hilum: A Case Report and Review of the Literature. Archives of Pathology & Laboratory Medicine. 2006;130(7):1049-52.
- Ghaouti M, Znati K, Jahid A, et al. Renal myelolipoma a rare extra-adrenal tumor in a rare site:a case report and review of the literature. Journal of Medical Case Reports. 2013;7:92.
- Hunter SB, Schemankewitz EH, Patterson C, et al. Extra-adrenal myelolipoma:a report of two cases. Am J Clin Pathol. 1992;97:402-04.
- Bishop E, Eble JN, Cheng L, et al. Adrenal myelolipomas show non-random X-chromosome inactivation in hematopoietic elements and fat: support for a clonal origin of myelolipomas. Am J Surg Pathol. 2006;30(7):838-43.
- Chang KC, Chen PI, Huang ZH, et al. Adrenal myelolipoma with translocation. Cancer Genet Cytogenet. 2002;134:77-80.
- Gierke E. Unusual myeloid tissue in the adrenal gland. Beitr Pathol Anat. 1905;7:311-25.
- Prahlow JA, Loggie BW, Cappellari GO, Scharhng JO, Teot A, Iskandar SS. Extra-adrenal myelolipoma: report of two cases South Med J 1995; 88(6):639-643.
- Xuefeng T, Minglu Y. Myelolipoma of the kidney:a seldom site for a ra6re extra-adrenal tumor. Journal of Medical Colleges of PLA. 2010;25(5):317–20.
- Beraha D, Block NL, Politano VA. Myelolipoma of the Kidney. Journal of Urology. 1974; 112:19-21.
- Clarke PE, Farver CR, Ulchaker JC, et al. A Rare Case of an Extra-Adrenal Myelolipoma Arising in the Renal Sinus:A Case Report and Review of the Literature. The Scientific World Journal. 2005;5: 109-117.
- Brietta L K, Watkins D. Giant extra-adrenal myelipoma. Arch Pathol Lab Med. 1994;118(2):188-190.
- Amin M B, Tickoo S K, Schultz D. Myelolipoma of the renal sinus an unusual site for a rare extra adrenal lesion. Arch Pathol Lab Med. 199l;123(7):631–34.
- Cox A, Offman S L, Merrimen JLO, et al. Bilateral renal myelolipomas. Can Urol Assoc J. 2010; 4(6):164-68.
- Ifazoglu N, Ureyen O, Keles M. Extra-adrenal myelolipoma with haemolytic anemia. Turkish Journal of Surgery. 2017;33(2):116-118.
- Bell D J, Amini B. Renal Angiomyolipoma Radiopaedia.
- Israel G M, Hindman N, Hecht E, et al. The use of opposed phase-chemical shift MRI in the diagnosis of renal angiomyolipomas. AJR Am J Roentgenol. 2005;184(6):1868-1872.
- Hora M, Hes O, Boudova L, et al. Well-differentiated liposarcoma of the kidney. British Journal of Urology International. 2002.