nutrition risk prevalence and nutrition care proposals for hospitalized and critically ill patients with covid19
Received: 02-Apr-2024 Editor assigned: 04-Apr-2024 Accepted Date: Apr 25, 2024; Reviewed: 06-Apr-2024 Revised: 10-Apr-2024 Published: 28-Apr-2024
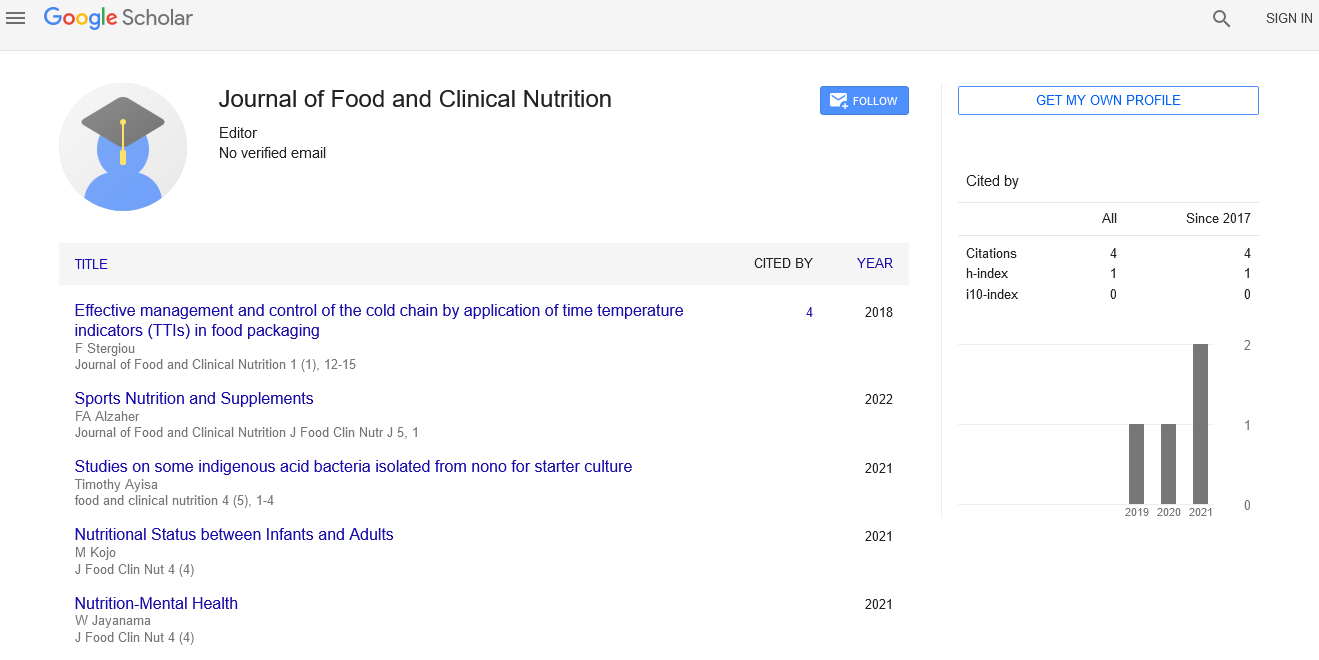
Citation: Roy S (2021) Nutrition Risk Prevalence and Nutrition Care Proposals for Hospitalized and Critically-Ill Patients with COVID-19. J Food Clin Nut Res. 4(4):1
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Introduction
Various constant infections or co-morbidities, including diabetes cardiovascular illness, influence over 70% of hospitalized grown-up patients and are regularly connected with expanded danger and pervasiveness of lack of healthy sustenance and more unfortunate results. The presence of comorbidities adds intricacy to addressing healthful requirements because of the cooperations of the sicknesses, illness state, and sustenance status. In hospitalized patients with co-morbidities, the medical services group regularly battles with focusing on dietary administration of the essential sickness while shuffling the basic wholesome requests of simultaneous infections. Perceiving wholesome danger in these patients is essential in mediating ahead of schedule to address healthful necessities that might affect results. Likewise, perceiving and treating healthful danger might assume a part in infection seriousness and results in hospitalized patients with COVID-19 who have different co-morbidities.
Description
Dietary danger and malnutrition in hospitalized and ICU patients with COVID-19 is common because of a few reasons including hyper metabolism brought about by aggravation, diminished food consumption, mechanical ventilation, GI bigotry, and different contraindications to nourishment support. Poor healthful status is connected to more terrible results in hospitalized COVID-19 patients, including mortality and expanded length of stay. Given the commonness of weight reduction and stoutness in the hospitalized COVID-19 patient populace, it is basic to distinguish those patients at wholesome danger for convenient execution of nourishment mediation. Nonetheless, nourishment hazard screening and appraisal in hospitalized patients, particularly right off the bat in the COVID-19 pandemic, represented a few difficulties. Chiefly, a restricted inventory of individual defensive gear made it hard for clinicians including dietitians to the go into rooms of patients in separation to gather screening and appraisal information. Access to patient rooms was frequently restricted to one medical services proficient, so dietitians were regularly dependent on other medical care suppliers, or relatives, or clinical history to gather applicable data. Dietary status is a frequently neglected part in irresistible sickness seriousness. Hospitalized or basically sick patients are at higher danger of malnutrition, and fast appraisal and therapy of poor healthful status can affect clinical results. As it identifies with the COVID-19 pandemic, an expected 5% of these patients expect admission to an ICU. Per clinical practice rules, nourishment treatment ought to be a center part of treatment regimens. By virtue of the earnest requirement for data identifying with the healthful help of these patients, clinical practice direction was distributed dependent on current basic consideration rules.
Conclusion
Dietary danger is exceptionally common in hospitalized COVID-19 patients. The etiology of nourishment hazard is multi-factorial and is reasonable because of a more older patient populace and high commonness of comorbidities joined with changed energy consumption auxiliary to expanded protein and energy needs because of fever, mechanical ventilation, weight and bulk misfortune, and hyper metabolism, and diminished supplement admission because of decreased craving, dyspnea, mechanical ventilation, and gastrointestinal narrow mindedness. Albeit clinical proof is missing to give explicit suggestions to nourishing administration in COVID-19 patients, experience from clinicians and rules identified with comparative illness states might fill in as an establishment until more clinical information is accessible. As more information arises in this populace, explicit suggestions and rules can be refreshed. Severely and fundamentally sick COVID-19 patients, those hospitalized or in an emergency unit, are at higher nourishing danger. Increased nutritional risk is associated with poorer clinical outcomes in these populations. Thus, quick assessment, identification, and treatment of poor nutritional status are vital for better clinical outcomes in harshly and critically ill COVID-19 patients.