Saphenion®: COVID-19, varicose veins and venous thrombosis
Received: 16-Mar-2021 Accepted Date: Mar 31, 2021; Published: 07-Apr-2021, DOI: 10.37532/1983-8905.2021.14(3).3-5
Citation: Zierau UT. Saphenion®: COVID-19, varicose veins and venous thrombosis. J Phlebol Lymphol. 14(3):12-14.
This open-access article is distributed under the terms of the Creative Commons Attribution Non-Commercial License (CC BY-NC) (http://creativecommons.org/licenses/by-nc/4.0/), which permits reuse, distribution and reproduction of the article, provided that the original work is properly cited and the reuse is restricted to noncommercial purposes. For commercial reuse, contact reprints@pulsus.com
Abstract
The risk factors for superficial vein thrombosis (OVT) are almost identical to those for Venous Thromboembolism (VTE) inthedeeplegandpelvicveins. However,the risk of superficial skin vein thrombosis is considerably higherif there are already varicosa veins. As can already be read everywhere, COVID-19 causes inflammation of the vascular wall of the deep leg veins. Considered on its own, this has a thrombogenic effect
Keywords
Varicose Veins; COVID-19 and vein wall inflammation; COVID-19 and venous thromboembolism
Introduction
The risk factors for superficial vein thrombosis (OVT) are almost identical to t those for Venous Thromboembolism (VTE) in the deep leg and pelvic veins. However, the risk of superficial skin vein thrombosis is considerably higher if there are already varicose veins [1-3].
Thisisduetothedefectivevenousvalves, throughwhichthevenous blood of the leg veins gets into the lower leg veins in a pathological alternating flow and return current! Thisreflux increases the pressure in the deep veins to over 120 mmHg-and with that alone there is a high risk of thrombosis.
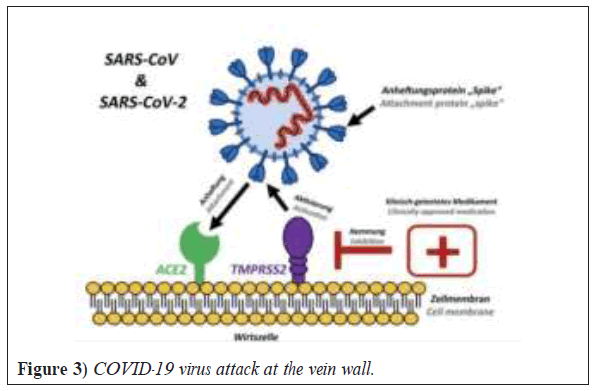
Now a virus is added, which obviously accumulates and multiplies in all the inner walls ofthelegveins. Thisalsoappliestothe vascular wall ofvaricose veins!
As can already be read everywhere, COVID-19 causes inflammation of the vascular wall of the deep leg veins. Considered on its own, this has a thrombogenic effect [4-7].
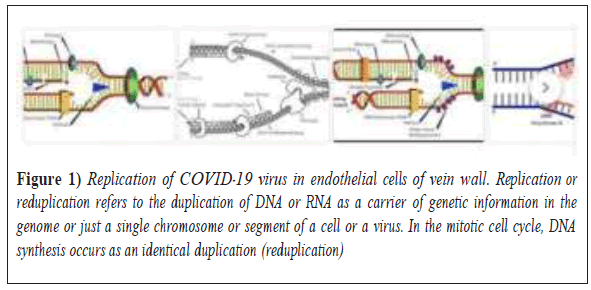
But this fact is not new: As COVID-19, also the flu virus, by the way-causes inflammation of the vascular wall of the deep leg veins. Considered on its own, this has a thrombogenic effect. These facts are known since 1970 (Figure 1) [8-10].
Figure 1: Replication of COVID-19 virus in endothelial cells of vein wall. Replication or reduplication refers to the duplication of DNA or RNA as a carrier of genetic information in the genome or just a single chromosome or segment of a cell or a virus. In the mitotic cell cycle, DNA synthesis occurs as an identical duplication (reduplication)
Varicose veins are the main cause of superficial vein thrombosis (OVT) of the lower extremities, but underlying diseases that already exist in parallel (e.g. autoimmune diseases, infections, malignancy or coagulation disorders) must also be looked for in superficial cutaneous vein thrombosis. A simultaneous deep vein thrombosis after cutaneous vein thrombosis of varicose veins occurs in 15% of all those affected. The severe complication pulmonary embolism can be seen in around 5% of those affected.
However, these numbers do not yet take into account the pathological influence of various viruses (such as flu viruses and COVID-19) [4-7,11-21] (Table 1).
| Male | Female | Complications |
|---|---|---|
| 44% | 76% | leg discomfort |
| 6% | 14% | phlebitis |
| 2% | 3% | pulmonary embolism |
| 56% | 55% | varicose vein |
| 20% | 11% | stem varicose veins |
| (Spider veins or reticular varices 3 times, 4 times more often than the trunk varicose) | ||
| Chronic venous insufficiency in 15% (same), From that 6% of them with skin changes and 1% with leg ulcers. | ||
| oldest Age dependency: | 5 times more often | complaintsphlebitis |
| 10 times more often | pulmonary embolismvaricose veinchronic venous insufficiency | |
TABLE 1 Results from Basler study-frequency of leg venous diseases in 4529 apparently healthy people
Many viral infections (flu, HIV, varicella, COVID-19) are associated with coagulation disorders. All aspects of the coagulation cascade, hemostasis, coagulation, and thrombosis dissolution can be affected. As a result, thrombosis and bleeding can occur in all vascular regions. The investigation of coagulation disorders as a result of various viral infections was not carried out uniformly. Commonpaths are thereforenot fullyunderstood. Formany severe viral infections, there is no other treatment than supportive measures. We have already suggested some ways of doing this
The question that must be asked here is whether the venous wall inflammation of the varicose vein does not exist first and whether the thrombosis of the varicose vein, which therefore quickly develops, migrates into the deep veins of the leg, which have already been damaged by the virus. This then leads to the often fatale pulmonary embolism, which is currently the case with COVID-19.
This pathological process in connection with viral infections was already discussed 50 years ago in connection with various flu pandemics and can be found in ourliteratureresearchinmanyolderscientificarticles(Figure 2 and 3).In our practices in Berlin/Rostock, several (5) patients between the ages of 43 and 67 with pronounced varicose veins have presented since mid-May 2020. In the medical history, pneumonia as a result of pulmonary embolism as a result of COVID-19 infection was found in all cases [13,17,18,22-25].
In our practices in Berlin/Rostock, several (5) patients between the ages of 43 and 67 with pronounced varicose veins have presented since mid-May 2020. In the medical history, pneumonia as a result of pulmonary embolism as a result of COVID-19 infection was found in all cases [13,17,18,22-25].
In the patient interview, our patients reported superficial venous thrombosis in the area of the varicose veins. In one case, a patient had undergone radical surgical varicose vein operation 7 years before the COVID-19 infection and suffered from recurrent varicose veins and phlebitis on the operated left leg. She then had to be treated with a deep vein thrombosis. The pneumonia set in about 14 days after the cutaneous vein thrombosis (phlebitis); she initially did not notice the pulmonary embolism. Whenshewas admittedtoa Berlin hospital, the COVID-19 infection was found.
The infection has now healed and the deep veins have been recanalized-we recommended that our patient rehabilitate the cutaneous vein system using VenaSeal®-vein glue and micro-foam therapy. This was then carried out on all five patients, in three cases both legs at the same time in August 2020– March 2021 using VenaSeal®-vein glue.
Recommendations
Saphenion®: COVID-19, varicose veins and venous thrombosis: Recommendations from a vascular surgical point of view
It is very important for us - as vascular surgeons - to point out that COVID-19 is not the first virus with these significant-sometimes fatal-side effects of thrombosis andpulmonaryembolism. There are other risk factors too.
And in any case, this also includes varicose veins, which are generally not considered so much from the point of view of illness. In terms of viral complications, these represent an easy target and are the cause of very rapid thrombosis and embolism [1,2, 9,13,16,20,22-24].
As a result, we urgently recommend our patients not only to address this problem in times of viral pandemics. Function and cosmetics are important factors, but complications asaresult of varicose veinscannot be safely and precisely planned or predicted! This results in the recommendation for specialist diagnosis and necessary therapy with the various therapy methods recommended today [9].
Saphenion: COVID-19, varicose veins and venous thrombosis: Recommendations of the professional associations
Inaddition to allthese aspects,doctorsneed tokeep aneye on something else. Inthecase of COVID-19,various mechanismscanleadtobloodcoagulation being disturbed. This can manifest itself in a pulmonary embolism, for example. In this complication, a blood clot obstructs one or more arteries in the lung.
Many of these thrombi, autopsy results suggest, have their origin in the deep leg veins. From there they are carried away with the bloodstream and flushed into the lungs and then, depending on the size of the clot, lay a pulmonary artery. As a result, the affectedlung sectionisunabletobreathe [23,24,26].
Depending on how big the blood vessel is that it is blocking in the lungs, an embolism can be fatal within a short time-this seems to be more common with COVID-19 than initially assumed. The risk of thrombosis and embolism in intensive care patients in hospital is 17%-47%.
The pulmonary embolism can also cause long-term damage. If it doesn’t resolve completely, it can lead to pulmonary hypertension. In this case, one must speak of long-term damage. The clot increases the resistance in the pulmonary circulation against which the heart has to pump. In the long run, the right ventricle of the heart is also increasingly overwhelmed, the patients are exhausted with the slightest exertion, gasping for air, complaining of water in their legs and dizziness. Life expectancy is also limited in many cases by pulmonary hypertension. All the involved German specialist societies involved (DGA, DGP, DGG) have now published therapy and prophylaxis recommendations. In view of the current data situation and the experience since 3/2020, active drug-based thrombosis prophylaxis and therapy is recommended for inpatients treated as well as for all those discharging from hospitals [27-30].
Conclusion
In addition, drug thromboembolism prophylaxis for people not suffering from COVID-19 with other risk factors (coagulation disorders, varicose veins, previous thrombosis or phlebitis, other infectious diseases) is also recommended for the duration of a completelockdown. The stay-at-home policyrequirespeopleto stayathomeforlongerperiodsoftime.Thismeans that inactivity andimmobility are pre-programmed and an increased risk of thrombosis/embolism is provoked. It is therefore important first of all to have a specialist examination and clarification of these risks and, if necessary, appropriate drug and physiotherapeutic thrombosis prophylaxis[31-33].
REFERENCES
- de Medeiros DM, Silva CA, Bueno C, et al. Pandemic influenza immunization in primary antiphospholipid syndrome (PAPS): A trigger to thrombosis and autoantibody production?. Lupus. 2014;23(13):1412-6.
- Khan R, Yasmeen A, Pandey AK, et al. Cerebral venous thrombosis and acute pulmonary embolism following varicella infection. Eur J Case Rep Intern Med. 2019;6(10).
- Zierau UT, Martel L, Lahl W. COVID-19 and Varicose Veins: Common Causes of Deep Vein Thrombosis and Embolism. J Phlebol Lymphol. 2020;13(2).
- Connors JM, Levy JH. COVID-19 and its implications for thrombosis and anticoagulation. Am J Hematol. 2020;135(23):2033-40.
- Decousus H, Epinat M, Guillot K, et al. Superficial vein thrombosis: Risk factors, diagnosis, and treatment. Curr Opin Pulm Med. 2003;9(5):393-7.
- Demelo-Rodríguez P, Cervilla-Muñoz E, Ordieres-Ortega L, et al. Incidence of asymptomatic deep vein thrombosis in patients with COVID-19 pneumonia and elevated D-dimer levels. Thromb Res. 2020;192:23-6.
- Maruyama H, Okugawa H, Takahashi M, et al. De novoportal vein thrombosis in virus-related cirrhosis: Predictive factors and long-term outcomes. Am J Gastroenterol. 2013;108(4):568-74.
- SaphenionPatientsInfo. COVID-19 and varicose. Saphenion. 2020.
- SaphenionPatientenInfo. COVID-19 Gefäßwandentzündung – So werden Thrombosen gemacht. Saphenion. 2020.
- How the coronavirus increases the risk of thrombosis. BMC. 2020.
- Filis K, Kavantzas N, Dalainas I, et al. Evaluation of apoptosis in varicose vein disease complicated by superficial vein thrombosis. Vasa. 2014;43(4):252-9.
- Gabrielli M, Lamendola P, Esperide A, et al. COVID-19 and thrombotic complications: Pulmonary thrombosis rather than embolism? Thromb Res. 2020;193:98.
- Wijarnpreecha K, Thongprayoon C, Panjawatanan P, et al. Hepatitis C virus infection and risk of venous thromboembolism: A systematic review and meta-analysis. Ann Hepato. 2017 Nov 6;16(4):514-20.
- Jerkic Z, Karic A, Karic A. Clinically silent deep vein thrombosis in patients with superficial thrombophlebitis and varicose veins at legs. Med Arch. 2009;63(5):288.
- Karathanos C, Spanos K, Saleptsis V, et al. Recurrence of superficial vein thrombosis in patients with varicose veins. Phlebology. 2016;31(7):489-95.
- Linnemann, Birgit. COVID-19: Update haemostaseologischer und vaskulärer Aspekte. Vasomed. 2020;32:233.
- Ramacciotti E, Agati LB, Aguiar VC, et al. Zika and Chikungunya virus and risk for venous thromboembolism. Clin Appl Thromb Hemost. 2019;25:1076029618821184.
- Tan BK, Mainbourg S, Friggeri A, et al. Arterial and venous thromboembolism in COVID-19: A study-level meta-analysis. Thorax. 2021.
- Tichelaar YV, Kluin-Nelemans HJ, Meijer K. Infections and inflammatory diseases as risk factors for venous thrombosis. Thromb Haemost. 2012;107(05):827-37.
- Warot M, Synowiec T, Wencel-Warot A, et al. Can deep vein thrombosis be predicted after varicose vein operation in women in rural areas? Ann Agric Environ Med. 2014;21(3).
- Van Rij AM, Chai J, Hill GB, et al. Incidence of deep vein thrombosis after varicose vein surgery. Br J Surg. 2004;91(12):1582-5.
- Kröger K. Stay at home – Politik und das Risiko venöser Thromboembolien. Vasomed. 2020;32:142–143.
- Saphenion. COVID-19, Krampfader und Venenthrombose. Saphenion. 2021.
- Das COVID-19 High Noon: Todesursache Schlaganfall, Thrombose, Lungenembolie/Update 11. Saphenion. 2020.
- Oliveira GN, Basso S, Sevivas T, Neves N. Varicella complicated by cellulitis and deep vein thrombosis. Case Reports. 2017.
- Thrombosen, Blutbild-und Hautveränderungen: EMA nimmt Stellung zu der Sicherheit von COVID-19-Vakzinen. Medscape. 2021.
- Saphenion®. COVID-19 Impfstoff Sputnik 5/update März 21. Saphenion. 2021.
- Goeijenbier M, Van Wissen M, Van De Weg C, et al. Viral infections and mechanisms of thrombosis and bleeding. J Med Virol. 2012;84(10):1680-96.
- Obi AT, Tignanelli CJ, Jacobs BN, et al. Empirical systemic anticoagulation is associated with decreased venous thromboembolism in critically ill influenza A H1N1 acute respiratory distress syndrome patients. J Vasc Surg Venous Lymphat Disord. 2019;7(3):317-24.
- Rieder M, Goller I, Jeserich M, et al. Rate of venous thromboembolism in a prospective all-comers cohort with COVID-19. J Thromb Thrombolysis. 2020;50(3):558-66.
- COVID-19. Das Thromboserisiko – Embolien? Saphenion. 2020.
- Miesbach W, Makris M. COVID-19: coagulopathy, risk of thrombosis, and the rationale for anticoagulation. Clin Appl Thromb Hemost. 2020;26:1076029620938149.
- Nicolaides A, Fareed J, Kakkar AK, et al. Superficial vein thrombosis. Clin Appl Thromb Hemost.2013;19(2):214-8.